INTRODUCTION
The surgical procedures used to reconstruct the aortic root are independent of morphological or etiopathogenic characteristics of the diseases that affect this aortic segment. The main conceptual difference of surgical techniques for aortic root lies in the use of a valved conduit or the aortic valve preservation, with their respective advantages and disadvantages. Since Bentall & De Bono [1] introduced the operation to replace the ascending aorta and the aortic valve for a valved conduit, several adaptations to this original technique have been proposed [2-5]. After mastering these operations, as an alternative, another concept for the treatment of this aortic segment arose, and it would be replaced associated with the aortic valve preservation.
Thus, it was believed that the complications related to anticoagulation could be avoided or reduced, whether they are thromboembolic or hemorrhagic, and infectious complications of patients undergoing the classic procedure. Sarsam & Yacoub [6] initially, and later, David & Feindel [7] have proposed techniques for aortic root reconstruction with the preservation of native aortic valve. In these patients, the valve leaflets do not show significant primary changes, but they may present secondary changes to the dilation of the aortic ring, in addition to abnormalities similar to those in the related aortic wall, which could limit the longevity of this procedure [8-10]. The native valve preservation, the main objective of any operation involving the heart valves, makes the procedure more laborious and time consuming, and does not ensure an early or late adequate result of the procedure (which usually occurs when using a valved conduit). Therefore, the purpose of this study is to analyze the early and late results of the aortic root reconstruction with a valved conduit, and with the aortic valve preservation.
METHODS
By reviewing the database of the Aorta Group Institute, the patients who underwent operation of aortic root reconstruction were identified, during November 2002 to September 2009. In this analysis, all patients who underwent elective or emergency procedures were included. Data were obtained by consulting the database, by reviewing medical charts and by telephone or letter, and by completing the specific questionnaire. The Institutional Ethics and Scientific Committee approved the condution of this work, with the research protocol No. 837/04.
We identified 164 patients, mean age 54 ± 15 years, 115 (70.1%) males and divided into two groups for analysis: those who underwent aortic root reconstruction with valved conduit and those who underwent radical resection of the ascending aorta with aortic valve preservation.
The epidemiological characteristics of these patients are presented in Table 1.
125 (76.2%) reconstructions were performed with valved conduit. 123 (98.4%) mechanical and two biological valves, 47 (37.6%) Bentall and De Bono classic operations, 67 (53.6%) Bentall and De Bono modified operations (button technique) and nine (7.2%) Cabrol operations. 39 reconstructions were also carried (23.8%) with the aortic valve preservation: 26 (66.6%) remodeling operations, as proposed by Sarsam & Yacoub [6], and 13 (33.3%) replantation operations, described by David & Feindel [7] (Table 2).
The patients defined as operated with acute and Stanford type A chronic aortic dissection, respectively those who were operated on the first 14 days of the acute event and those operated after 14 days.
The late follow-up period with echocardiographic restudy was performed in 88% of patients and the mean follow-up was 41 ± 21 months.
Statistical analysis
Survival curves and event-free survivals were estimated by the Kaplan-Meier method. The associations of potential risk factors for survival were evaluated by log-rank test and the Cox proportional model (risk factors for reoperation could not be determined by low occurrence). The groups were compared using the chi-square test for categorical variables and runk-sum for continuous variables. Data were expressed as mean ± standard deviation, statistical significance was
P < 0.05 and the significance for survival was evaluated with a 1-sample log-rank test.
RESULTS
Hospital mortality was 4.9% (8 / 164), 5.6% (7 / 125) in operations with the valved conduit and 2.6% (1 / 39) in the ascending aorta reconstructions with the aortic valve preservation (
P <0.05).
There were 127 aneurysms, six (4.7%) deaths, and 37 dissections with two (5.4%) deaths, 9 of them were acute and 28 were chronic.
The hospital deaths were due to septic shock in three (1.8%) patients, bleeding in two (1.2%), ventricular fibrillation in two (1.2%) and acute heart failure in one (0.6%) patient with early endocarditis of the aortic prosthesis. The immediate postoperative complications were 15 (9%), reoperations for bleeding,13 (8%) patients presented acute atrial fibrillation, 12 (7%) required permanent pacemaker, 10 (6%) initially had low cardiac output, two (1.2%), cerebrovascular accidents (CVA), two (1.2%), episodes of ventricular tachycardia, and one (0.6%), myocardial infarction.
During the study period (1233 ± 720 days), there were nine deaths, three secondary to myocardial infarction, two to cerebral infarction, one to thrombosis of the aortic prosthesis, one to pancreatic cancer and two with unknown cause. Among the followed-up patients, 98.4% were in functional class I and II (88% of the sample). The main late complications are detailed below.
The survival rate in seven years for patients undergoing aortic root reconstruction with a valved conduit was 77.6% (95% CI = 62.3% to 92.9%) and those undergoing reconstruction with aortic valve preservation was 93.5% (95% CI = 84.5% to 100%). There was no significant difference between the two forms of treatment (
P = 0.1) (Figure 1).

Fig. 1 - Survival curves of patients undergoing aortic root reconstruction with valved conduit (VC) and the aortic valve preservation, during a seven-year follow-up period
Three reoperations were performed during the follow-up period, one in those patients whose valve was preserved (remodeling operation) for important symptomatic aortic insufficiency four years after the operation, one underwent reconstruction with the valved conduit for aortic prosthetic endocarditis six years after surgery. The third valve replacement was necessary for mitral valve insufficiency in patients with typical anomalous papillary insertion from patients with Marfan syndrome, six years after the operation to preserve the aortic valve.
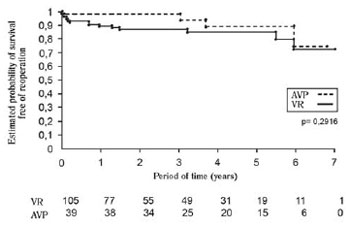
The reoperation-free survival in the seven-year follow up for patients undergoing the aortic root reconstruction with a valved conduit was 72.1% (95% CI = 56.1% to 88.1%) and those undergoing reconstruction with aortic valve preservation was 74.4% (95% CI = 45.5% to 100%). There was no difference between the two groups (
P = 0.2916) (Figure 2).
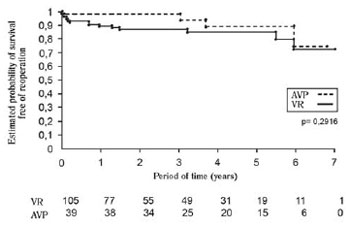
Fig. 2 - Free survival curves of reoperation in patients undergoing aortic root reconstruction with valved conduit (TV) and the aortic valve preservation, during a seven-year follow-up period
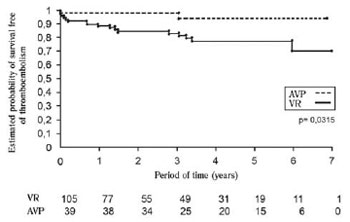
The reoperation-free survival in the seven-year follow up for patients undergoing the aortic root reconstruction with a valved conduit was 70.7% (95% CI = 54.5% to 86.9%) and those undergoing reconstruction with aortic valve preservation was 93.5% (95% CI = 84.5% to 100%).
The hemorrhagic complications free-survival in the seven-year follow up for patients undergoing the aortic root reconstruction with a valved conduit was 59.0% (95% CI = 44.4% to 73.6%) and those undergoing reconstruction with aortic valve preservation was 93.5% (95% CI = 84.5% to 100%); significantly lower for patients receiving oral anticoagulants (
P = 0.0012). Complications related to chronic use of oral anticoagulation occurred in 16 patients who had received a valved conduit. There were three major and 13 minor hemorrhages, taking into consideration that one patient died of cerebral hemorrhage (Figure 4).
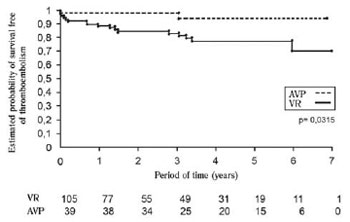
Fig. 3 - Free survival curves of thromboembolic complications in patients undergoing aortic root reconstruction with valved conduit (VC) and the aortic valve preservation, during a seven-year followup period

Fig. 4 - Free survival curves of bleeding complications in patients undergoing aortic root reconstruction with valved conduit (VC) and the aortic valve preservation, during a seven-year follow-up period
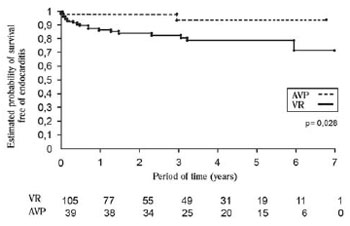
The endocartitis free-survival in the seven-year follow up for patients undergoing the aortic root reconstruction with a valved conduit was 71.2% (95% CI = 55.2% to 87.2%) and those undergoing reconstruction with aortic valve preservation was 93.5% (95% CI = 84.5% to 100%); significantly lower for patients receiving the valvular prosthesis (
P = 0.0028). Five patients with prosthetic valve endocarditis presented the resolution of the infectious condition only with drug treatment (Figure 5).
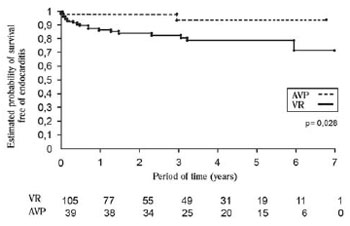
Fig. 5 - Free survival curves of endocarditis patients undergoing aortic root reconstruction with valved conduit (TV) and the aortic valve preservation, during a seven-year follow-up period
Predictors of hospital and late mortality determined by univariate analysis are detailed in Table 3. The multivariate analysis showed that creatinine greater than or equal to 1.4 mg / dl showed an OR of 6 (95% CI = 1.8 to 19.5,
P <0.003), the Cabrol operation showed an OR of 12 (95% CI = 3-50, P <0.0004) and renal dialysis showed an OR of 16 (95% CI = 3.6 to 71,
P <0.0002) (Table 3). Both in univariate and multivariate analysis predictors of the need for reoperation were not identifid, during the follow-up period.
DISCUSSION
The operations for the aortic root reconstructions have already been widely used, as their immediate and late results are known, as well as a greater technical difficulty of carrying out the to preserve the aortic valve.
In this study, we observed a low mortality of these operations. The difference in results observed between the operations with the valved conduit and the aortic valve preservation do not allow us to state that, one type of operation overlaps the other, because the groups are not similar and the aortic valve preservation is not a operation for all patients. In any manner, the complications related to the chronic use of oral anticoagulation (thromboembolic and / or hemorrhagic phenomena) and prosthetic valve infection should be taken into consideration when choosing an operation against another.
Wannamathee et al. [11] also observed that the elective aortic root reconstruction has reduced mortality, especially when compared to urgent or emergency interventions. In a multicenter study, 675 patients with Marfan syndrome who underwent reconstruction with a valved conduit showed hospital mortality of 1.5% in elective cases, 2.6% for urgent cases and 11.7% in the emergency rooms. In multivariate analysis, the Cabrol operation was significant to decrease the late survival. In our study, this change was mainly due to the fact that we used this surgical technique in cases of reoperation, and "per se" should justify the worst result. Other variables, such as reduced ejection fraction, aortic regurgitation severity and increased left ventricular cavity were not predictors of late mortality.
Apart from the low occurrence, we observed no difference in the reoperation of our patients, regardless of operation carried out for the aortic root reconstruction, differently from what other authors has presented. The probable reason due to the strict selection of patients for the aortic root reconstruction with valve preservation, the low number of procedures in the aortic leaflets, external fixation of the commissural pillars when using the remodeling technique and the follow-up time relatively short for the study patients [12].
Ergin et al. [13] reported significant reduction in reoperation rate and increased survival in patients undergoing operation with a valved conduit when used the technique proposed by Kouchoukos Button et al. [5]. Svensson et al. [14] did not need to reoperate any patient in his sample. Savunen & Aho [15] performed angiography in 53 of the 60 patients studied, three years after the operation with a valved conduit, and faced no problem in coronary ostial anastomoses. Niederhäuser et al. [16], with seven reoperations in 181 patients operated with a valved conduit, did not identify predictors for the need of reoperation. On the other hand, Zehr et al. [17] in a series of 203 surgical patients observed that Marfan syndrome, root reconstruction with the aortic valve preservation and the need of associated valvular procedure were significant predictors for necessity of reoperation.
Yacoub et al. [18] observed 11% of reoperation in a ten-year follow-up with series of 158 patients who underwent remodeling technique, especially due to secondary aortic insufficiency to late dilation of the aortic ring. David et al. [19] showed that in 151 patients who underwent aortic root reconstruction with the aortic valve preservation, the reoperation-free survival of the aortic valve was 99.1% for reimplantation technique and 97, 2% for the remodeling technique in an eight-year follow up period. Nevertheless, the severe aortic insufficiency-free survival during the study period was different when compared to both techniques, with 90.3% for the reimplantation technique and 55.6% for the remodeling technique.
The fixation of the aortic ring was considered as the main reason for the lowest incidence of reoperation in patients who underwent reimplantation technique when compared to remodeling technique [12,18-22]. Several other technical changes were suggested for the reconstruction process of the aortic root with valve preservation and were summarized by Miller [23] in the editorial referred above.
It has been shown that surgical manipulation of one or more aortic leaflets aiming to a better coaptation is related to the increased need for valve reoperation in the late follow-up of these patients [24]. In our study, only six (15%) patients required valve procedure associated with the manipulation of the aortic valve, with good results until this moment of the follow-up period.
The valve preservation in patients with Marfan syndrome is another point of contention. Although the aortic valve leaflets are often functionally normal, they are structurally compromised. Missirlis et al. [8] observed that the length of the aortic valves leaflets in Marfan syndrome is greater than the normal ones. It was also demonstrated that the abnormal fibrillin metabolism affects the valvar tissue in these patients. Fleischer et al. [10] also showed that the aortic and mitral valve leaflets are equally affected by the fragmentation of fibrillin-1, as well as the aortic wall, and these changes are more intense when patients are older than 20 years. In this report, 11 patients with Marfan syndrome underwent aortic root reconstruction with valve preservation, without the need for reoperation. Oliveira et al. [22] reported that 61 patients with Marfan syndrome underwent reconstruction with the aortic valve preservation and present 100% survival free of reoperation in 10 years. However, 25% already present from moderate to severe aortic valve insufficiency.
As patients with Marfan syndrome, patients with bicuspid aortic valve, despite the morphological changes of the leaflets, had good results, similar to those obtained in trivalvular patients [25].
Oliveira et al. [22] also observed that the aortic valve leaflets, in general, appeared to be normal when the aneurysm was shorter than 5 cm and only 50% of them appeared to be normal when the aneurysm had between 5 and 6 cm. On the other hand, in patients with aneurysms larger than 6 cm, most of the leaflets was abnormal, being more recommended the replacement of the root for the valved conduit.
The ring size also seems relevant when choosing the operative technique. Aortic rings larger than 25 mm before the root reconstruction were significant predictor for the need of reoperation [23]. Casselman et al. [26] reported that a 27 mm ring or larger can be a predictor of recurrent aortic insufficiency in bicuspid aortic valve repair.
Due to what we observed and the difficult access of the brazilian population to adequate health care in the long-term period, it seems a problem to the aortic root reconstruction with a valved conduit, especially by the continued use of oral anticoagulants. Six (4.8%) of our patients had thromboembolic events during the follow-up period and one of them resulted in death. Kouchoukos et al. [5], dealing with patients whose medical care is considered superior to the reality of third world countries as Brazil, also observed a significant incidence of problems related to inadequate anticoagulation. There were thromboembolic complications in 18% of patients in the twelve-year follow up. Hemorrhagic complications are also a reality for patients using oral anticoagulants. Sixteen (12.8%) of our patients had hemorrhagic complications, with one death of cerebral hemorrhage.
The infectious complications are more frequent when the native valve is not preserved. In our sample, the presence of six (4.8%) patients with valve infection could have resulted in greater need for reoperation, if the therapeutic success with drug treatment of prosthetic valve endocarditis had not been so high.
The late mortality of these patients is low, similar to the life expectancy of the general population, as demonstrated previously [17]. Renal failure, being dialytic or not, it is a factor that is invariably associated with higher mortality, either early or late. In this study, the Cabrol operation was also presented as a predictor of mortality, although it is important to mention not because of the operation itself, but due to the fact that it is performed in patients at higher operative risk (reoperations).
Despite the indisputable results of operation for the aortic root reconstructions with a valved conduit, complications from the use of mechanical valve prosthesis are not negligible, especially for the reality in our public health system. The entire procedure can be done with similar results to those obtained with the valved conduit preserving the native valve and it should be stimulated, even if it is not a procedure either for all surgeons or all patients. [27,28].
In conclusion, we can state that the aortic root reconstruction has a low early and late mortality, a high survival free of complications and little need for reoperation. During the late follow-up, the aortic root reconstruction with preservation of the aortic valve showed a lower incidence of bleeding, thromboembolic events and endocarditis.
REFERENCES
1. Bentall H, De Bono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23(4):338-9. [MedLine]
2. Grey DP, Ott DA, Cooley DA. Surgical treatment of aneurysm of the ascending aorta with aortic insufficiency. A selective approach. J Thorac Cardiovasc Surg. 1983;86(6):864-77. [MedLine]
3. Lewis CT, Cooley DA, Murphy MC, Talledo O, Vega D. Surgical repair of aortic root aneurysms in 280 patients. Ann Thorac Surg. 1992;53(1):38-45. [MedLine]
4. Cabrol C, Pavie A, Gandjbakhch I, Villemot JP, Guiraudon G, Laughlin L, et al. Complete replacement of the ascending aorta with reimplantation of the coronary arteries: new surgical approach. J Thorac Cardiovasc Surg. 1981;81(2):309-15. [MedLine]
5. Kouchoukos NT, Wareing TH, Murphy SF, Perrillo JB. Sixteen-year experience with aortic root replacement. Results of 172 operations. Ann Surg. 1991;214(3):308-18.
6. Sarsam MA, Yacoub M. Remodeling of the aortic valve anulus. J Thorac Cardiovasc Surg. 1993;105(3):435-8. [MedLine]
7. David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. 1992;103(4):617-21.
8. Missirlis YF, Armeniades CD, Kennedy JH. Mechanical and histological study of aortic valve tissue from a patient with Marfan's disease. Atherosclerosis. 1976;24(1-2):335-8. [MedLine]
9. Segura AM, Luna RE, Horiba K, Stetler-Stevenson WG, McAllister HA Jr, Willerson JT, et al. Immunohistochemistry of matrix metalloproteinases and their inhibitors in thoracic aortic aneurysms and aortic valves of patients with Marfan's syndrome. Circulation. 1998;98(19 Suppl):II331-7.
10. Fleischer KJ, Nousari HC, Anhalt GJ, Stone CD, Laschinger JC. Immunohistochemical abnormalities of fibrillin in cardiovascular tissues in Marfan's syndrome. Ann Thorac Surg. 1997;63(4):1012-7. [MedLine]
11. Gott VL, Greene PS, Alejo DE, Cameron DE, Naftel DC, Miller DC, et al. Replacement of the aortic root in patients with Marfan's syndrome. N Engl J Med. 1999;340(17):1307-13. [MedLine]
12. Dias RR, Mejia OV, Carvalho EV Jr, Lage DO, Dias AR, Pomerantzeff PM, et al. Aortic root reconstruction through valve-sparing operation: critical analysis of 11 years of follow-up. Rev Bras Cir Cardiovasc. 2010;25(1):66-72. [MedLine] View article
13. Ergin MA, Spielvogel D, Apaydin A, Lansman SL, McCullough JN, Galla JD, et al. Surgical treatment of the dilated ascending aorta: when and how? Ann Thorac Surg. 1999;67(6):1834-9.
14. Svensson LG, Longoria J, Kimmel WA, Nadolny E. Management of aortic valve disease during aortic surgery. Ann Thorac Surg. 2000;69(3):778-83.
15. Savunen T, Aho HJ. Annulo-aortic ectasia. Light electron microscopic changes in aortic media. Virchows Arch A Pathol Anat Histopathol. 1985;407(3):279-88. [MedLine]
16. Niederhäuser U, Künzli A, Genoni M, Vogt P, Lachat M, Turina M. Composite graft replacement of the aortic root: long-term results, incidence of reoperations. Thorac Cardiovasc Surg. 1999;47(5):317-21. [MedLine]
17. Zehr KJ, Orszulak TA, Mullany CJ, Matloobi A, Daly RC, Dearani JA, et al. Surgery for aneurysms of the aortic root: a 30-year experience. Circulation. 2004;110(11):1364-71. [MedLine]
18. Yacoub MH, Gehle P, Chandrasekaran V, Birks EJ, Child A, Radley-Smith R. Late results of a valve-preserving operation in patients with aneurysms of the ascending aorta and root. J Thorac Cardiovasc Surg. 1998;115(5):1080-90. [MedLine]
19. David TE, Ivanov J, Armstrong S, Feindel CM, Webb GD. Aortic valve-sparing operations in patients with aneurysms of the aortic root or ascending aorta. Ann Thorac Surg. 2002;74(5):S1758-61.
20. Birks EJ, Webb C, Child A, Radley-Smith R, Yacoub MH. Early and long-term results of a valve-sparing operation for Marfan syndrome. Circulation. 1999;100(19 Suppl):II29-35. [MedLine]
21. Kallenbach K, Hagl C, Walles T, Leyh RG, Pethig K, Haverich A, et al. Results of valve-sparing aortic root reconstruction in 158 consecutive patients. Ann Thorac Surg. 2002;74(6):2026-32.
22. Oliveira NC, David TE, Ivanov J, Armstrong S, Eriksson MJ, Rakowski H, et al. Results of surgery for aortic root aneurysm in patients with Marfan syndrome. J Thorac Cardiovasc Surg. 2003;125(4):789-96. [MedLine]
23. Miller DC. Valve-sparing aortic root replacement in patients with the Marfan syndrome. J Thorac Cardiovasc Surg. 2003;125(4):773-8. [MedLine]
24. Burkhart HM, Zehr KJ, Schaff HV, Daly RC, Dearani JA, Orszulak TA. Valve-preserving aortic root reconstruction: a comparison of techniques. J Heart Valve Dis. 2003;12(1):62-7. [MedLine]
25. Nazer RI, Elhenawy AM, Fazel SS, Garrido-Olivares LE, Armstrong S, David TE. The influence of operative techniques on the outcomes of bicuspid aortic valve disease and aortic dilatation. Ann Thorac Surg. 2010;98(6):1918-24.
26. Casselman FP, Gillinov AM, Akhrass R, Kasirajan V, Blackstone EH, Cosgrove DM. Intermediate-term durability of bicuspid aortic valve repair for prolapsing leaflet. Eur J Cardiothorac Surg. 1999;15(3):302-8. [MedLine]
27. Subramanian S, Borger MA. Aortic valve reconstruction: current status. Herz. 2010;35(2):88-93. [MedLine]
28. Albes JM. Aortic valve reconstruction: why, when and how? Thorac Cardiovasc Surg. 2010;58(2):61-8. [MedLine]
Article receive on Monday, August 16, 2010


 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license