INTRODUCTION
Lindberg et al. [1] in 1986 demonstrated the inhibitory effect of the H/K pump in the gastric parietal cells in reducing the acidity of gastric juice and in the treatment of peptic ulcer. Later, other H/K pump inhibitors have been developed, including the Lansoprazole, Pantoprazole, Rabeprazole, and Tenatoprazole [2]; the most frequent prescribed one being the omeprazole.
Although they have been developed with specific therapeutic intent to treat gastric hyperacidity, in recent years proton pump inhibitors were associated with benefits in the treatment of angina pectoris and myocardial ischemia, considering that chest pain may mimic the gastroesophageal reflux symptom from coronary artery disease, and the esophagitis pain may also be enough to motivate stress ischemia and cardiac pain in patients suffering from both diseases. That is why it has been described that the treatment of gastroesophagitis has reduced the frequency of angina attacks [3-5].
Other important evidence suggesting the protective effect of omeprazole on coronary ischemia is the fact that its administration has reduced the frequency of both anginal attacks and electrocardiographic signs of myocardial ischemia during exercise treadmill tests in studies of coronary heart disease patients [6]. However, there are still no specific experimental demonstrations showing the clinical hypotheses of its protective effect on coronary ischemia-reperfusion.
Another very important evidence suggesting the protective effect of omeprazole on the purpose of this research constitutes analyze the effects of omeprazole in protecting myocardial contractility in isolated rat hearts subjected to ischemia-reperfusion.
The aim of the present study was to analyze the effects of omeprazole on the protection of myocardial contractility of isolated hearts of rats submitted to the ischemia-reperfusion lesion.
METHODS
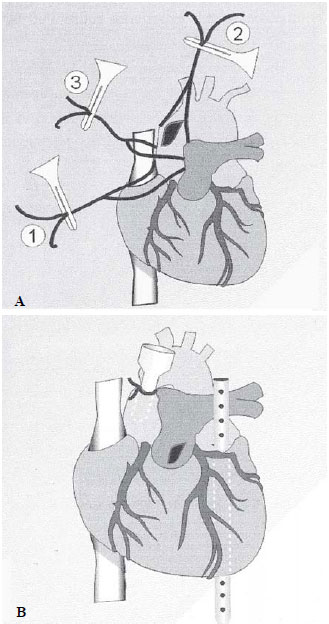
The study was approved by the Local Institutional Ethics Committee. We studied 12 Wistar rats without distinction of sex with an average body weight of 280 g. After anesthesia ketamine and xylazine in a 10 mg and 2 ml intra-abdominal dose intravenous, respectively, is administered. The animals underwent a wide range median thoracotomy and 500 IU of heparin were regularly injected into the right atrium. For safety and quickness in the procedure preparation, the ascending aorta was isolated with the 3-wire technique [7]. The first wire pulls and lifts the aortic root to protect of the cusps and to prevent ventricular cannulation; the second wire pulls and lifts the cranial (superior) end of the ascending aorta; and the third wire is passed between the first two, to tie off the aorta on the cannula after it was inserted (Figure 1A and B). A perfusion cannula was introduced and secured in the ascending aorta, preventing injury to the aortic cups to ensure adequate coronary perfusion; then the left atrium was opened and a multiperforated cannula inserted and externalized our push out through the left ventricle apex. Finally, the pulmonary artery was opened at its origin to facilitate the drainage of the right ventricle.
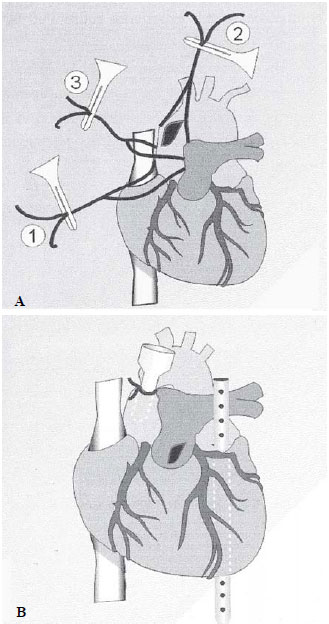
Fig. 1 - A: Aortic isolation for cannulation; B: Cannulationz of the aorta and left ventricle
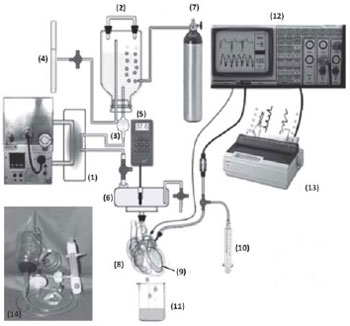
The hearts were removed, at a maximum of a 3-minute time after the procedure. They were reperfused with Krebs-Henseleit solution (aered/gassed with 95% O2 and 5% CO2, at 37°C, using a modified, disposable Langendorff system, model-FCSFA ServCor, Comex Ind. & Com Ltda) (Figure 2) with circulation system and water heating and telethermometer models (Braile Biomédica Ltd), biomonitor BESE®, and a matricial printer Epson®. After ten minutes of coronary reperfusion, the transventricular catheter was removed, and a pre-calibrated balloon catheter was introduced into the left ventricle.
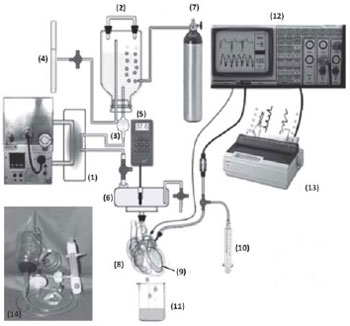
Fig. 2 - Diagram of the Study System of an Isolated Heart. 1. Termal exchanger, 2. Perfusate reservoir. 3. Microfilter (20 ì), 4. Gauge/Manometer, 5. Telethermometer, 6. Chamber, 7. Carbogen (95% 02 +5% C02), 8. Heart, 9. Intraventricular balloon, 10. Drug injector, 11. Flow Collector, 12. ECG and Ventricular Pressure monitor, 13. Printer, 14. Disposable set
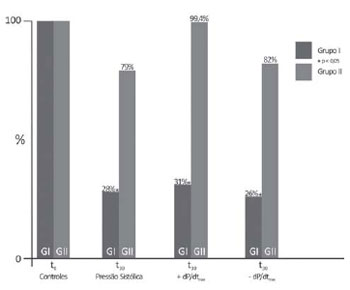
All hearts studied presented normal parameters of myocardial contractility (after a 10-minute recovery all hearts presented systolic pressure less than or equal to 110 mmHg, diastolic pressure of 8 mmHg. The control register (t0) was obtained at the 15th minute of recovery. The six hearts of the group I (GI) underwent 20 minutes of ischemia and 30 minutes of reperfusion. In six hearts of group II (GII), immediately before ischemia, 200 mcg of omeprazole and H/K ATPase pump blocker of more frequent clinical use in our environment was administered through coronary perfusion (Figure 3).
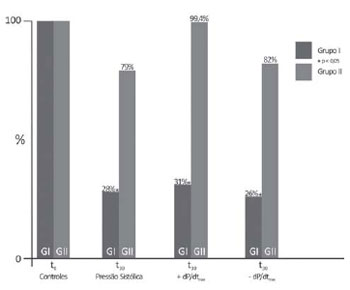
Fig. 3 - Percentage of systolic pressure variation, +dP/dt
max; and -dP/dt
max.
The following parameters were controlled after the stabilization period (t0) and after a 30-minute period past coronary reperfusion was initiated (t
30): heart rate (HR/bpm), coronary flow (CFo/ mL/min), systolic pressure (mmHg), +dP/dt
max and -dP/dt
max (mmHg/s).
We used the Kruskal-Wallis nonparametric statistical analysis. All p vales < 0.05 were considered statistically significant.
RESULTS
No differences (P > 0.05) were found between HR and CFo in both groups (Table 1). At the end of reperfusion period (t
30), the reduced SP changes were significant (P <0.05) with averages ranging from 138 ± 14.7 mmHg (t0) to 38 ± 14.4 mmHg (t
30). These were equivalent to the initial value (28.0 ± 3.6%) (t0) of Group I, which ranged from 140 ± 15.6 mmHg (t0) to 112 ± 25 mmHg (79.0 ± 5.9%) in Group II (t
30); the +dP/dt
max declined to 31.0 ± 5.6% at t
30 (t0 annd t
30 were 3328 ± 996 and 1187.4 ± 449.6 mmHg/s, respectively) in GI, remaining at 99.4 ± 11.2% (P < 0.05) in GII at t
30 (t0 3374 ± 1247 mmHg; t
30 3141 ± 1681.1 mmHg/s). The -dP/dt
max declined to 26.0 ± 7.3% (t0 = 1859 ± 203.9; t
30 407 ± 284.1) in GI, remaining at 82.0 ± 2.2% in GII (P < 0,05) (t0 = 1859 ± 203.9 mmHg/s; t
30 = 1570 ± 515.7 mmHg/s) (Table 2 and Figure 3).
DISCUSSION
In 1994, Nagashima et al. [8] were also the first to demonstrate the existence of the proton pump H
+/K
+ ATPase in the myocardium as well. They studied their electrophysiological interference in the hearts of guinea pigs [9], motivating further research, such as the multicenter trials GUARDIA and ESCAMI. These trials have carefully analyzed inhibitors such as eniporide and cariporide - the proton pump Na
+/H
+ blockers -, emphasizing the protection against myocardial ischemia-reperfusion injuries, but with contrasting results and doubts about the prophylactic effect and indication of its therapeutic use [10]. More recently, Budzynski et al. [6], in 2008, described the beneficial effects of omeprazole in the protection of anginal attacks and ischemic electrocardiographic changes during the exercise test in patients with coronary heart diseases.
In the present study, it was found a significant protection of omeprazole against ischemia-reperfusion in isolated rat hearts, with reduced +dP/dt and -dP/dt to 31 ± 5.6% and to 26 ± 7.3 %, respectively, on average after 30 minutes of postischemic reperfusion in Group I (control), and mean values of +dP/dt and -dP/dt of 99.4 ± 11.2% and 82 ± 2.2%, respectively, in Group II with administration of 200 mcg of omeprazole pre-ischemia. These results associate the benefits of omeprazole with the results reported by studies addressing myocardial protection with ischemic preconditioning [11-15]. The pharmacokinetics basis may be related to changes in transmembrane H
+/K
+ gradients, the first markers of myocardial ischemia, responsible for the repolarization expressed in T-wave morphology of the electrocardiogram [16]. In 1998, the studies by Hotta et al. [17] in isolated hearts of guinea pigs, using an analytic method for detecting fluorescent compounds, the fluorometry and magnetic resonance imaging, indeed confirmed the acute ionic intracellular changes of the myocardial ischemia-reperfusion with changes in pH and concentrations of cytosolic N+, H+, and Ca+, thus confirming the blockade and protection by omeprazole as well.
Additional studies may precisely determine the interaction of proton pump blockers with the phenomena of ischemic myocardial pre- and post-conditioning, with a potential favorable resolution for both clinical therapeutic and preventive use in coronary heart diseases as well as in the myocardial protection for cardiac surgeries. In this respect, the preconditioning by H+/K+ pump blockers preoperatively can optimize the cardiac protection, replacing intermittent occlusions of the coronary arteries or the aorta itself, with a parietal harmful potential whose efficacy had already been refuted [18], and differing from the conclusion of the present study, which establishes a significant protection of myocardial contractility
REFERENCES
1. Lindberg P, Nordberg P, Alminger T, Brändström A, Wallmark B. The mechanism of action of the gastric acid secretion inhibitor omeprazole. J Med Chem. 1986;29(8):1327-9. [MedLine]
2. Sachs G, Shin JM, Howden CW. Review article: the clinical pharmacology of proton pump inhibitors. Aliment Pharmacol Ther. 2006;23(Suppl 2):2-8. [MedLine]
3. Libby P, Bonow RO, Mann DL, Zipes DP. Braunwald's heart disease. Philadelphia:Saunders;2008.
4. Dobrzycki S, Baniukiewicz A, Korecki J, Bachórzewska-Gajewska H, Prokopczuk P, Musial WJ, et al. Does gastroesophageal reflux provoke the myocardial ischemia in patients with CAD? Int J Cardiol. 2005;104(1):67-72. [MedLine]
5. Gomes OM, Faraj M. Cardiologia da família. 1ª ed. Belo Horizonte:Edicor;2005.
6. Budzynski J, Klopocka M, Pulkowski G, Suppan K, Fabisiak J, Majer M, et al. The effect of double dose of omeprazole on the course of angina pectoris and treadmill stress test in patients with coronary artery disease: a randomised, double-blind, placebo controlled, crossover trial. Int J Cardiol. 2008;127(2):233-9. [MedLine]
7. Gomes OM, Gomes ES, Carvalho JI, Faraj M. Adaptações técnicas na preparação de Langendorff para estudo de corações isolados de pequenos animais. Coração. 1999;9:36-8.
8. Nagashima R, Odashiro K, Morita S. Evidence for the existence of myocardial H+-K+ATP and its electrophysiological effects. Jpn Heart J. 1994;35(suppl):473-4.
9. Nagashima R, Tsuda Y, Maruyama T, Kanaya S, Fujino T, Niho Y. Possible evidence for transmembrane K(+)-H+ exchange system in guinea pig myocardium. Jpn Heart J. 1999;40(3):351-64. [MedLine]
10. Avkiran M, Marber MS. Na(+)/H(+) exchange inhibitors for cardioprotective therapy: progress, problems and prospects. J Am Coll Cardiol. 2002;39(5):747-53. [MedLine]
11. Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74(5):1124-36. [MedLine]
12. Zhao ZQ, Corvera JS, Halkos ME, Kerendi F, Wang NP, Guyton RA, et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285(2):H579-88. [MedLine]
13. Gomes OM, Valladares UF, Santos CH, Abrantes RD. Preconditioning abolishion by midazolam in isolated hearts of rats. Acta Cir Bras. 2009;24(3):173-6. [MedLine]
14. Pinheiro BB, Fiorelli AI, Gomes OM. Efeitos do pós-condicionamento isquêmico na função ventricular esquerda de corações isolados de ratos. Rev Bras Cir Cardiovasc. 2009;24(1):31-7. [MedLine] View article
15. Oliveira DM, Gomes ES, Mussivand T, Fiorelli AI, Gomes OM. Efeitos da N-acetilcisteína no precondicionamento isquêmico: estudo em corações isolados de ratos. Rev Bras Cir Cardiovasc. 2009; 24(1):23-30. [MedLine] View article
16. Gomes OM, Gomes ES, Faraj M. Doença da discinesia miocárdica de estresse. Rev Bras Cir Cardiovasc. 2004;19(4):378-85. View article
17. Hotta Y, Fujita M, Nakagawa J, Ando H, Takeya K, Ishikawa N, et al. Contribution of cytosolic ionic and energetic milieu change to ischemia- and reperfusion-induced injury in guinea pig heart: fluorometry and nuclear magnetic resonance studies. J Cardiovasc Pharmacol. 1998;31(1):146-56. [MedLine]
18. Pêgo-Fernandes PM, Jatene FB, Kwasnicka K, Hueb AC, Gentil AF, Coelho FF, et al. Influência do pré-condicionamento isquêmico na proteção miocárdica em revascularização do miocárdio com pinçamento intermitente da aorta. Rev Bras Cir Cardiovasc. 2001;16(1):7-13.
Article receive on Tuesday, June 15, 2010
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license