President: Euríclides de Jesus Zerbini.
Participantes: A. de Carvalho Azevedo (Guanabara), Cid Nogueira (Porto Alegre), Domingos Junqueira de Moraes (Guanabara), Hugo João Felipozzi (São Paulo), Delmont Bittencourt (São Paulo), Adib D. Jatene (São Paulo) & Jesse Teixeira (Guanabara).
EXPERIENCE IN CARDIAC SURGERY WITH CARDIOPULMONARY BYPASS: STUDY OF A SERIES OF 1000 OPERATED CASES
E. J. ZERBINI
CARDIOVASCULAR SURGERY IN BRAZIL
Between July 1958 and April 14, 1963, a group of 1,000 patients underwent cardiac surgery with extracorporeal circulation, being 680 patients in the Hospital das Clinicas of the Faculty of Medicine, University of São Paulo and 320 patients in the Institute of Cardiology of the State of São Paulo. In this group are not included aortic aneurysms operated with partial perfusion without the use of the oxygenator.
Perfusions were performed through a set of artificial heart-lung machine consisting of occlusive pump and disks oxygenator type Kay-Cross. The overall mortality in this series was 11.3%, having declined 25% in the first hundred cases to 7% in the last hundred. In the first patients, we observed mortality directly related to the perfusion process, with prolonged anoxic cardiac arrest, observing several cases of complete atrioventricular block. These complications disappeared gradually and mortality came to have a direct relationship with the severity of the condition being corrected. When we started the corrections of tetralogy of Fallot and complex mitral lesions, the mortality rate rose again. With experience, there were fewer complications in these cases.
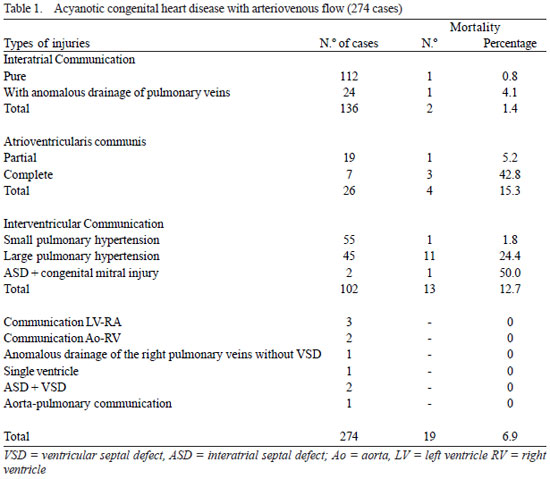
In the four following tables are exposed the main cardiopathies undergoing correction, using cardiopulmonary bypass.
Symposium held during the XIX Brazilian Congress of Cardiology in Salvador, Bahia, on 07/18/1963.
1. In the first group (table 1) are exposed 274
acyanotic congenital heart diseases with arteriovenous flow; mortality was 6.9%. Among interauricular communications, only at the beginning of our experience we lost two cases (1.4%), being 1 in the group of 112 simple lesions and 1 in the group of 24 lesions associated with anomalous pulmonary veins.
Among 26 patients with
atrioventricularis communis the mortality rate was 15.3%, being higher in the overall shape of the deformity, when there is an associated VSD. In the partial order, with cleft of the mitral or tricuspid valve, one patient died among 19 patients operated.
In a group of 102 VSD, we observed 12.7% mortality, with 24.4% in the 45 cases with high pulmonary hypertension and only l, 8% in the group of 55 cases with mild pulmonary hypertension. In two cases of ventricular septal defect associated with congenital mitral lesions there was one death.
In this group are also three cases of communication between the left ventricle and the right atrium, 2 cases of communication between the aorta and the right ventricle, 1 case of anomalous drain of the right pulmonary veins without interatrial communication, a case of single ventricle, 2 cases of interatrial and interventricular communications associated and one case of aortic-pulmonary fistula.
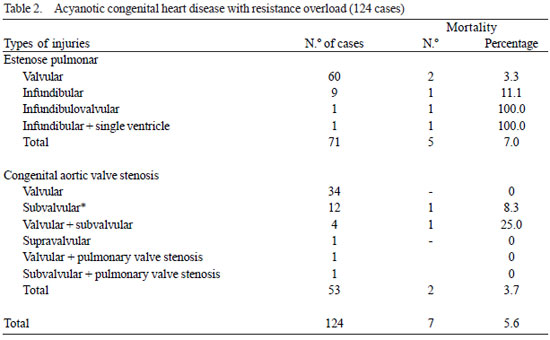
2. In Table 2 there is a study of 124
acyanotic congenital heart diseases with overhead resistance, with overall mortality of 5.6%.
In the group of 71 pulmonary stenosis, the mortality was 7%, being higher in the infundibular stenosis. We counted 11 cases of simple infundibular stenosis or associated with other injuries, 3 deaths were subsequent to aortic clamping without draining the left atrium, performed in the first cases operated in 1958. After the systematic draining of the left atrium in these cases, mortality disappeared. Among 60 pulmonary valve stenosis we observed two deaths.
In the group of 53 congenital aortic stenosis there were only two deaths (3.7%), counting 34 valve stenosis, 12 subvalvular, 4 valvular and subvalvular and 2 cases of association of aortic and pulmonary stenosis.
Four patients underwent cardiotomy, and we found no injury susceptible to surgical correction.
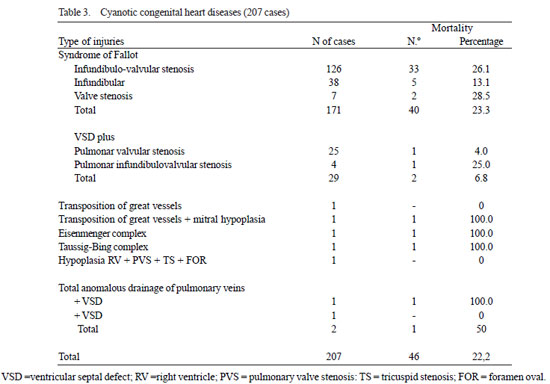
3. Table 3 shows a study of 207 cases of cyanotic congenital heart disease undergoing cardiopulmonary bypass.
In a group of 171 patients with Fallot's syndrome, we had 23.3% mortality, noting that this mortality is higher in patients with infundiibulovalvular pulmonary stenosis associated with ventricular septal defect. Recently, thanks to the introduction of some technical details in the correction of infundibular stenosis and the postoperative treatment, we have had better results in this group of patients.
As for the so called trilogy of Fallot, i.e., association of ventricular septal defect and pulmonary stenosis, we counted 29 cases with 2 deaths (6.8%).
This group consists of 25 cases of valvular pulmonary stenosis and 4 cases of infundibulovalvular stenosis associated with ventricular septal defect.
Two cases of complete transposition of great vessels underwent palliative operations. In one of them, it was found a very small foramen ovale and extreme pulmonary valvular stenosis, this lesion was partially relieved and the atrial septum widely open, the patient had a satisfactory outcome. The second patient had a small interatrial communication and mitral valve atresia, communication has been expanded, but the patient died after surgery.
In a case of Eisenmenger complex, we tried to close the interventricular communication, expecting that cyanosis were produced by the dextroposition of the aorta and not by the lung resistance; this patient, however, died by respiratory failure.
Another patient, patient with Taussig-Bing complex, underwent cardiotomy, but no correction was possible. We also had two cases of total anomalous drain of the pulmonary veins.
In the group of cyanotic congenital heart disease, mortality was 22.2%.
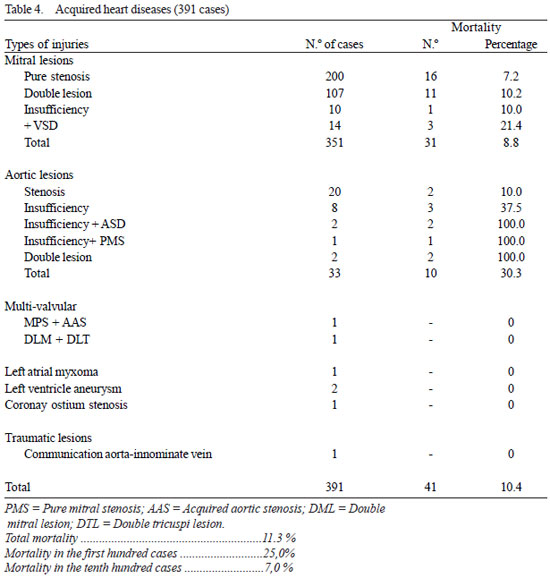
4. In Table 4 are gathered 391 cases of acquired heart diseases. Among 351 lesions of the mitral valve we had the overall mortality rate of 8.8%, being 7.2% in pure mitral stenosis, 10.2% in the double mitral lesions, 10.0%, insufficiencies in pure mitral lesions and 21.4% in mitral lesions associated with interatrial communication.
Initially, we only performed the operation with cardiopulmonary bypass in cases of complex mitral lesions, such as reoperations, in the presence of calcium in the mitral valve, when there was associated mitral regurgitation in the presence of atrial fibrillation or previous embolism, suggesting left atrial thrombosis, and also in children, who may be carriers of congenital mitral stenosis. Currently, the group of uncomplicated pure stenoses, we have excellent results without complications.
Acquired aortic lesions are more complex than congenital, with several cases requiring replacement of the valve leaflets by plastic Hufnagel. The overall mortality in this group was 30%.
We have avoided operations in multivalvular injuries. Only in two cases the correction was performed with good results: one with mitral and aortic valve stenosis and another with double mitral and tricuspid valve lesion.
Other less common injuries are listed in Table 4: There was a myxoma of the left atrium, 2 left ventricular aneurysms, one case of ostial stenosis of the coronary arteries by atheroma and a traumatic fistula between the aorta and innominate vein.
Conclusions - The bypass procedure is safe for the correction of many congenital and acquired heart diseases. In this series of 1,000 cases, total mortality was 11.3%, being 7% in the last hundred cases. This mortality is related to the complexity of the condition being corrected, being minimal in less complex heart diseases. The experience has allowed expanding the indications for surgery to treat increasingly complex lesions, which until now could not be corrected.
INDICATIONS OF SURGICAL TREATMENT IN CYANOTIC CONGENITAL HEART DISEASE
A. DE CARVALHO AZEVEDO
Facing a congenital heart disease it will not be amenable to surgery only in two circumstances: 1) when there is still not a surgical technique that may benefit the patient: in this case are the holders of common arterial trunk, single ventricle with large pulmonary circulation and aortic atresia; 2) when the evolution or the stage reached by the disease no longer allows surgical treatment: in this group are included heart diseases with abnormal communication between the arterial and venous sector (at auricular, ventricular or pulmonary levels), with large pulmonary hypertension and pure or predominant venoarterial shunt.
Virtually every other heart surgery is now possible, either palliative or curative. Consider some of the important ones:
Transposition of great vessels - besides Baffes' technique, although difficult, it was beneficial in some cases; recently it was proposed by Ochsner a palliative procedure, with the creation of large interatrial communication, using the technique of Blalock and Hanlon. They selected patients with severe anoxemia, with or without heart failure. Among 28 operated patients, most under 12 months, 82% survived the operation with sheer improvement.
Tricuspid atresia - in cases with decreased pulmonary blood flow, palliative surgery is possible, either by creating an aortopulmonary anastomosis, or by creating a cavapulmonar anastomosis.
Cyanosis and anoxemia may also be alleviated in several other complex malformations of the heart, by the creation of a right aortapulmonar anastomosis directly or through a subclavian artery. It is important in order to indicate anastomoses of this type; the presence of great anoxemia with pulmonary hypotension and pulmonary arteries. In this group we can mention: single ventricle, levocardia, isolated dextrocardia, pulmonary stenosis with ventricular septal defect associated with corrected transposition of great vessels.
In the trilogy of Fallot, the surgery referral is formal, being possible complete correction.
In anomalous connections of the great vessels with cyanosis, there are also surgical means of returning the patient to normal.
Finally, the tetralogy of Fallot, i.e., that group of cases with pulmonary stenosis, ventricular septal defect and cyanosis. We have to analyze it into two subgroups: a) infants and children less than four years, b) over four years old.
In group
a one should resort to palliative surgery and not the total correction with cardiopulmonary bypass. This indication is based mainly on the high mortality with total correction, either due to the small circulating blood volume either due to the small caliber of the pulmonary vessels and the right ventricle, or, finally, by the inability of the pulmonary vascular bed (source of thrombosis and recanalization) to support a normal blood flow.
Thus, even today, it is necessary that the cardiovascular surgeon is accustomed to the techniques of Blalock-Taussig and Potts and be able to perform them in the cyanotic infant carrier of tetralogy of Fallot. Long-term reviews evidence that palliative surgery for patients with this anomaly, by the technique of Brock, Potts or Blalock-Taussig, when performed in patients over eight years old, produces lasting results, although in younger patients the benefit is not permanent and it should be admitted the palliative technique as a first approach for subsequent total correction.
In group
b, cyanotic patients with tetralogy of Fallot over four years of age there is indication for total correction of defects with cardiopulmonary bypass, unless associated lesions or atypical symptoms make preferable the anastomotic surgery. The angiocardiographic or cine-angiocardiographic study is, in this group of patients, the most important method to confirm the diagnosis and surgical indication.
INDICATIONS FOR SURGICAL TREATMENT OF CONGENITAL HEART DISEASE BEFORE THE AGE OF TWO YEARS
CID NOGUEIRA
Congenital heart defects are a major cause of mortality in early childhood. A survey done by the U.S. Dept. of Health Education and Welfare, showed that in that nation, 7,000 children die every year, victims of congenital heart disease before one year of age, 88% of them yield during the first six months of life . Keith et al. reported that in the Hospital for Sick Children in Toronto, congenital heart defects are the leading cause of mortality.
The development and progress of modern cardiovascular surgery created new perspectives in the treatment of these configurations.
Some cardiac defects such as aortic atresia are incompatible with life. Autopsies practiced in several series of children, however, reveal that the cardiac defects most often responsible for death are likely to curative or palliative surgical treatment at that age, with reasonable success.
Considering the comments, we can state that the surgical treatment of congenital heart disease is indicated for small size patients less than two years of age or 10 kg, where clinical manifestations are severe and uncontrollable by hospitalization and medical treatment. We prefer to intervene, whenever possible, after the patient develops more physically and is older.
We can group the pathophysiological mechanisms by which cardiac defects cause the death of two main types: those that lead to heart failure and those that produce anoxia.
Heart failure can arise from the difficulty of emptying one of the ventricles (systolic overload of the pulmonary and aortic stenosis or of a coarctation). The most frequently noted, however, as a cause of uncontrollable heart failure is the presence of a large systemic-pulmonary shunt with large increase of flow in small circulation and high output heart failure. This is the kind of heart failure associated with ventricular septal defect and patent ductus arteriosus (PDA).
Severe anoxia, with or without the cyanotic crises, is another complication of intracardiac malformations, that commonly produces the patient's death within the first months or years of life. The pathophysiological mechanisms by which anoxia (cyanosis) is produced are:
a) The presence of an intracardiac venoarterial shunt (ASD or VSD) in association with a low-flow pulmonary circulation secondary to stenosis or pulmonary atresia. Tetralogy of Fallot is the malformation most often seen as responsible for this type of hemodynamic disorder, consisting of 75% of cases of cyanotic congenital heart disease.
b) The presence of independent systemic and pulmonary circulation (transposition of great vessels), being life only possible as a result of mixing of arterial and venous blood, which takes place through septal associated malformations (VSD, ASD). The transposition of the great vessels is a congenital heart disease most often responsible for death in infancy. Keith noted that 86% of these patients succumb during the first six months of life, 52% die before one month of age.
The analysis of the results achieved by surgery and the comparison of the results obtained in patients not treated surgically allows us to continue indicating palliative operations (lower risk), and corrective actions, with or without the use of cardiopulmonary bypass for cases of symptomatic congenital heart disease with severe clinical symptoms, cyanosis or failure in patients who have not yet reached the age of two.
Cardiopulmonary bypass and the magnitude of the surgery performed for complete correction of intracardiac malformations elevate the risk of this treatment in patients of small size. We illustrate our commentary with the following fact: Cooley et al. operated 157 children with VSD, between 2 and 9 years old, with a mortality of 5.7%. The same authors reported a mortality rate of 42% in 31 patients with VSD operated with one year old or less.
We tried to avoid, whenever possible, the use of cardiopulmonary bypass in a patient of small size and indicate preferably curative operations (ligation of the ductus arteriosus, resection of coarctation of the aorta, pulmonary valvotomy) or palliative operations (systemic-pulmonary anastomosis, pulmonary artery banding, Blalock-Hanlon operation and superior vena cava anastomosis with the right pulmonary artery) that did not require the use of perfusion.
Our experience in the Department of Thoracic and Cardiovascular Surgery of the University of Medicine in Porto Alegre, with surgical treatment of congenital heart disease before the age of two, consists of 21 patients operated from January 1962 to April 1963. Surgery was indicated when in the presence of heart failure uncontrolled by medical therapy or severe anoxia, with or without cyanotic crisis.
HEMODILUTION PROBLEMS IN CARDIOPULMONARY BYPASS
DOMINGOS JUNQUEIRA MORAIS
The possibility to perform extracorporeal circulation with intentional hemodilution could theoretically provide several advantages: it would avoid blood incompatibility, reducing blood traumatism and decrease blood viscosity. All these factors would contribute to make the infusion easier and safer.
In Brazil, to our knowledge, there was only the work of Sergio Paladino et al., Demonstrating that mechanical hemolysis was reduced by dilution in physiological solution or plasma. Following this principle, we chose as diluents substances, initially, plasma and Dextran, because they are the ones that came closest to the physiological conditions.
We verified experimentally, using high flows, that the dilution could be very severe, reducing the hemoglobin rate to 3.5 to 4g/100ml, with no noticeable signs of hypoxia, and while we had definitive survival in animals perfused until for 4 hours.
Dilution with Dextron presented with the inconvenience of determining tendencies for bleeding. However, in clinics, used in quantities between 300 and 500g, it was satisfactory.
Our first patient operated on in June 1960, was a case of tetralogy of Fallot, perfused for 2 hours and 35 minutes. In this patient, hemoglobin decreased to 6g/100ml, hematocrit to 25% and pH remained normal throughout the perfusion period, this patient has recovered and is in excellent condition. Later, we began to use the method in all our cases, making changes in substances and diluents aiming to reduce to 1000-1200 ml the fluid needed to fill up the pump-oxygenator system.
We use as diluents substances, citrated plasma, Hemoderivate conserved plasma in pure form or mixed with Dextran or dextrose solution.
In 15 patients, we used Ringer solution plus a phial of Hemoderivate serum albumin. No differences in these types of dilution were observed.
In 85 patients, this method was used for surgery of congenital and acquired lesions, with a mortality of 20.5%. Normothermia was employed with high flow: 60 to 80ml/kg/min in adults and 100-120ml/kg/min in children.
Over the past eight months we have been using the same method with moderate hypothermia, reduced flow and, preferably, dextrose solution and Ringer's solution to fill up the pump-oxygenator system, as recommended by Zudhi et al.
We have employed flow of 35-40ml/kg/min for adults and 40-60ml/kg/min for children with hypothermia 25-30ºC. Using this technique, 46 patients were operated, eight deaths occurred, i.e., 17% mortality.
We believe that moderate hemodilution with hypothermia offers more advantages: possibility to reduce the perfusion flow, contributing to further reduce blood trauma, makes the management of infusion simpler, provides greater safety when performing cardiac arrest during surgery. Furthermore, hemodilution, besides the advantages already mentioned, lowering blood viscosity, helps to make the heating and cooling faster and uniforms, thus avoids or reduces the phenomenon of stacking of red blood cells, which is one of the drawbacks of hypothermia and probably increases the oxygen consumption of the plasma, improving the perfusion of vital organs.
Thus, hemodilution and hypothermia complement one another as fusion techniques and are currently the method of our choosing.
IMMEDIATE AND LATE RESULTS OF SURGICAL CORRECTION OF VENTRICULAR COMMUNICATIONS
HUGO JOÃO FELIPOZZI
Our presentation is restricted to the assessment of immediate and late results of surgical correction of ventricular communications, practiced by the staff of the Institute of Cardiology Sabbado D'Angelo, from 1957 to April 1963.
Fifty-six patients with ventricular septal defects, isolated or associated with other cardiac defects, underwent 58 operations with cardiopulmonary bypass (2 reoperations).
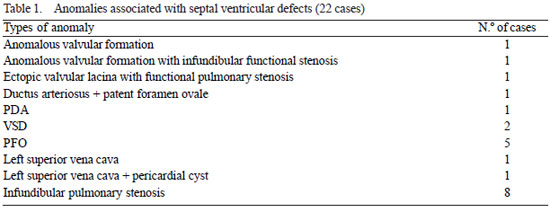
Of the 56 cases, 34 had isolated lesions and 22 had one or more anatomical or functional associations (Table 1).
Of the 22 patients with associated injuries, 8 had infundibular pulmonary stenosis. The criterion used to classify them among the ventricular communication was the presence of normal arterial saturation. The cases of ventricular communication with infundibular pulmonary stenosis and arterial unsaturation are not included in this series, because we consider them as a syndrome of Fallot. The patients' ages ranged between 2 and 36 years, and the age group 20-10 years presented the highest number of cases (32).
In order to undergo surgery, all patients underwent complete clinical cardiological examination, performing cardiac catheterization in 49 cases, with or without selective angiocardiography.
Based on the hemodynamic studies, patients were classified into four groups: A) Pressure in the pulmonary artery to 50% of the systemic pressure with left-right pure shunt: 24 cases. B) Pulmonary artery pressure between 50 and 85% of the systemic pressure with left-right pure shunt: 7 cases. C) Pulmonary artery pressure between 85 and 100% of the systemic pressure, with predominant left-right shunt: 5 cases. D) Pressure in the pulmonary artery between 85 and 100% of the systemic pressure, with predominant right-left shunt: 4 cases. In 9 patients the pulmonary artery was not catheterized, which is why such cases were not included in the classification.
For correction of intracardiac defects, we seek, whenever possible, avoid opening the ventricle. Thus, it was the transauricular tract used in 34 cases with tricuspid valve section in 6. The transventricular access was used 19 times. In three cases, the approach was combined: auriculotomy plus ventriculotomy. In one case it was performed ventriculotomy plus pulmonary arteriotomy. In a reoperation of high septal defect, we used the transaortic tract with hypothermic cardiac arrest (icing on the heart).
In the initial phase of our experiment, we used the cardioplegia induced by potassium citrate, soon abandoned by the known drawbacks. Subsequently, we adopted the intermittent aortic clamping. Currently, we prefer to correct ventricular communicationS with the heart stopped in selective hypothermia applying ice over the heart.
The ventricular septal defects were corrected, in most cases, with plastic grafts of Teflon or compressed Ivalon. It was performed in just a few simple sutures with separate stitches. In the intraoperative and postoperative complications, we initially considered the most serious, which led to death and then, minor complications.
In the series of 56 patients undergoing 58 interventions, there were 10 deaths, all hospital deaths and there were no late deaths. Four deaths were the result of serious surgical accidents: a) laceration of superior vena cava before the establishment of cardiopulmonary bypass; b) Abbot filter clogging, interposed in the arterial circuit, c) postoperative bleeding through the puncture of the aorta for induction of cardioplegia with potassium citrate, d) accidental section of the venous brachiocephalic trunk in one case of reoperation.
Excluding such cases of serious accidents at the beginning of our experience with cardiopulmonary bypass, the analysis of the obituary went on to demonstrate a close correlation between the degree of pulmonary hypertension and mortality. Thus, the remaining six deaths occurred among 10 patients classified in groups C and D, i.e., pulmonary artery compression between 85% and 100% of the systemic pressure, and crossed shunt.
From February 1959, 27 consecutive patients with pulmonary pressure values below 85% of the systemic pressure (groups A and B) had their defects corrected without death.
Among the complications of lesser consequence should be highlighted: a) total temporary atrioventricular block, occurring in 5 cases, b) signs of heart failure, of major or minor degree, in 8 patients, 2 of which it was confirmed persistent left-right shunt (both reoperated with good results in one case), in other cases, heart failure could be controlled clinically, c) postoperative bleeding, with reopening of the chest in two patients, d) acute renal failure in one case, with full recovery after the use of artificial kidney; e) signs of transient cerebral anoxia due to inadequate perfusion in all three cases recovered and normal f) the serious pulmonary complications, in the beginning of our experience with cardiopulmonary bypass stopped since the systematic use of continuous decompression of the left cardiac cavities during cardiopulmonary bypass. Those that occurred afterwards were inherent to the pulmonary hypertension.
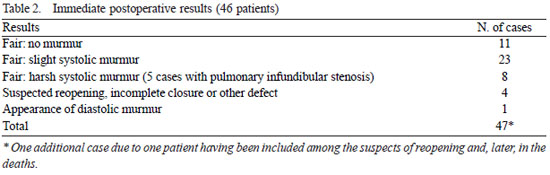
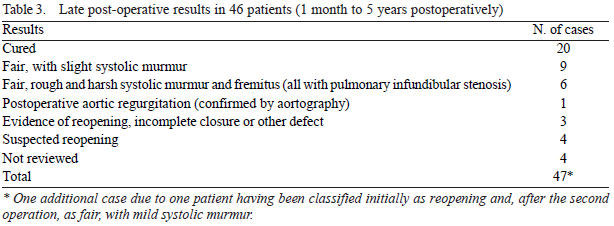
The early and late postoperative results of 46 survivors, observed for periods varying from 1 month to 5 years are presented in tables 2 and 3.
We recatheterized only seven patients, being confirmed the persistent of left-right shunt in three cases, being higher than in the preoperative in two of them, yet, there was in both reduction of pressure in the right ventricle. In a fourth case suspect of reopening, the catheterization was normal.
In two cases there was normalization of pulmonary pressures, and in one there is persistent moderate hypertension. The patients who still show any radiological alteration or murmur accompanied by fremitus were labeled as suspects of reopening and must be recatheterized. We excluded only those patients holding infundibular pulmonary stenosis, in which the persistence of harsh murmur with fremitus is the rule in our experience.
In summary, our study confirms the close correlation between the degree of pulmonary hypertension and pulmonary vascular resistance and the surgical outcome achieved. Such verification will require the increasingly stringent selection of candidates for correction of ventricular septal defects, which is not justified in our opinion, at present, to continue recommending surgery in cases in Group D, i.e., predominant left-right shunt. The selection of patients is the most important factor for obtaining good results with minimal surgical risk, as demonstrated by the absence of mortality in 27 patients with pulmonary pressure less than 85% of the systemic pressure and pure left-right shunt.
SURGICAL TREATMENT OF MITRAL VALVE HEART DISEASES WITH CARDIOPULOMONARY BYPASS
DELMONT BITTENCOURT
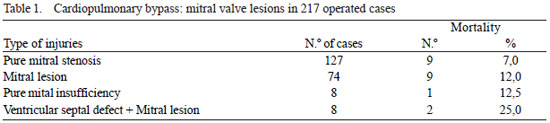
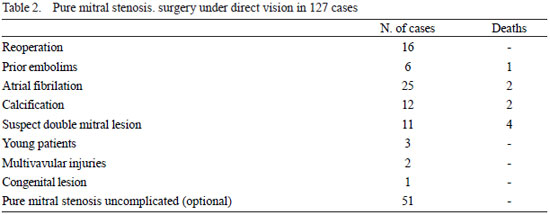
This report refers to the experience of the Hospital das Clinicas of the Faculty of Medicine, University of São Paulo, concerning the surgical treatment of 217 consecutive cases of lesions of the mitral valve operated between May 1959 and April 1963. This series includes 127 cases of pure stenosis, 74 cases of mitral lesion, 8 cases of pure mitral insufficiency and 8 cases of interatrial communications associated with mitral valve lesions.
Immediate mortality was 9 cases between pure mitral stenosis (7%), 9 cases between the double mitral lesions (12%), one case between the pure mitral insufficiency (12.5%) and one case among the ventricular septal defects associated mitral lesions (25%). The overall mortality in this series was 9.7% (21 cases). Of those deaths, 18 occurred in the first hundred operated cases (18%) and three occurred among the 117 remaining cases (2.5%).
Two cases of multivalvular injuries were operated and, in both, the lesions were corrected in one surgery. One of them had pure mitral stenosis associated with rheumatic aortic stenosis and the other showed an association between mitral stenosis and double tricuspid lesion.
The approach was the anterior lateral right thoracotomy with resection of the anterior arch of the fourth rib. In one case, in which the mitral stenosis was associated with aortic stenosis, it was used the medium-sternal tract 1. The cases of pure mitral stenosis were referred to surgery because they presented one or more of the following complications: 1) reoperation, 16 cases, 2) prior embolism, 6 cases, 3) atrial fibrillation, 25 cases, 4) calcification evidenced by planigraphy, 12 cases, 5) suspected mild mitral regurgitation, 11 cases; 6) younger patients with less than 12 years old, for possible congenital lesion of the mitral valve, 3 cases; 7) Multivalvular lesions, 2 cases.
Since November 1961, we began to operate under direct vision all complicated cases of mitral stenosis, and not just the cases complicated by the factors listed above. It was thus abandoned the classical or closed surgery, for non-complicated cases of mitral stenosis. The results of this conduct, adopted in 51 cases, were extremely favorable so far, especially for aestetacustical signs and radiological, electrocardiographic and vetorcadiographic regression. No deaths occurred in this group of 51 patients.
The surgery of mitral stenosis under direct vision allows wide opening of the commissural fusion. Thus, disappearing the occurrence of partially open valves, which is common in closed surgery of mitral stenosis.
Only two cases presented unicommissural stenosis, being the latter duly corrected. The treatment of subvalvular lesions is undoubtedly more perfect under direct vision.
In 70% of the cases it has been conducted a longitudinal section of the anterior papillary muscle, of the posterior, or both. The dilatation of the conglomerate and retracted chordae tendon is also possible under direct vision, and consequently achieving better mobility of the valvular apparatus. This is one of the strongest arguments for the use of open surgery in all cases of mitral valve lesions, especially those not complicated, as we do today.
Mitral stenosis was accompanied by severe calcification in 12 cases of this series, with two deaths. In these fatal cases, the valve was too injured and it would admit indication for total replacement.
Eleven patients with mitral stenosis were suspected to have associated mitral regurgitation. These cases were revealed during surgery as pure stenosis, accompanied by functional tricuspid insufficiency. Four deaths occurred among these patients.
Three children under 12 years of age, the youngest, 9 years, were operated without mortality. In all these cases, the mitral valve showed a suggestive appearance of rheumatic lesion. In contrast, a patient of 20 years with mitral stenosis presented during surgery, an appearance highly suggestive of congenital mitral valve lesion. Finally, one patient of 32 years of age, holding severe kyphoscoliosis of the spine, had a preoperative diagnosis of pure mitral stenosis, the surgical exploration of the mitral valve and the tricuspid valve revealed valve apparatus anatomically and functionally normal.
2. Seventy four cases of mitral lesion were operated with cardiopulmonary bypass. In such cases, the valvular damage is more pronounced with regard to fibrosis, the incidence of calcification and retraction of the tendinous chordae. Nine deaths (12%) occurred in this series.
In most cases of mitral lesion, the correction of valvular stenosis and the release of this chordae, followed often by the section of the papillary muscles, were sufficient to control the presence of mitral regurgitation. However, in 21 cases (28%), it became necessary to use a partial prosthesis of Ivalon of Teflon to correct mitral regurgitation.
3. Eight cases of pure mitral insufficiency were operated with one death (12.5%). The process of surgical treatment of most of these cases was that of circumferential reduction of the mitral annulus dilated by unipolar or bipolar fusion.
4. Eight cases of mitral valve lesions associated with ventricular septal defect (VSD) were operated with cardiopulmonary bypass. In all of them, the valvular lesion has been corrected by the transseptal tract after right atriotomy. The mitral lesion associated with VSD was pure stenosis in 2 cases, double mitral lesion in 4 cases and pure mitral regurgitation in 2 cases. None of these cases gave impression of congenital mitral lesion, they all seem rheumatic lesions.
CONCLUSIONS
1. All mitral injuries must have surgical indication for repair under direct vision using cardiopulmonary bypass.
2. The pure stenotic lesions without complications showed no mortality in a series of 51 cases operated in the open. The stenotic lesions complicated by calcification, atrial fibrillation, previous embolism or restenosis, showed mortality of 12%. The overall mortality for mitral stenosis was 7%.
3. Some cases of multivalvular injuries allow simultaneous treatment of injuries, as for example, the association of mitral stenosis and aortic stenosis, or a combination of mitral and tricuspid lesions.
4. The double mitral lesions present valves more intensely affected by fibrosis and calcification. About 10% of these cases should undergo valve replacement by total prosthesis; however, we still possess no fully satisfactory prosthesis. Partial prosthesis were used in 28% of cases of double mitral lesion.
5. The mitral lesions associated with VSD were stenotic in only 25% of cases. In most patients (75%), there is the presence of a major or minor degree of mitral regurgitation.
6. The overall mortality in this series of 217 cases was 9.7%. The mortality in the last 117 operated cases was 2.5%.
RESULTS OF THE SURGICAL TREATMENT OF AORTIC VALVE LESIONS
ADIB D. JATENE
In the period between March 1961 and March 1963 were operated at the Department of Surgery of the Institute of Cardiology in Sao Paulo State, 37 patients with aortic injuries. Thirty-four had stenosis and 3 had aortic insufficiency.
The distribution of the cases of stenosis, according to the location, was as follows: one patient had supravalvular stenosis, 11 patients had valvular stenosis by commissural fusion, calcium-free, 11 patients had valvular stenosis by commissural fusion and calcification more or less extensive; 6 cases had subvalvular stenosis, alone, 4 cases presented valvular and subvalvular stenosis, 1 case had muscular stenosis.
The indication for operation was done by determining the gradient between the left ventricle and the aorta in 10 cases. In the remaining 24 cases, the indication was based on clinical, radiological and electro and vectorcardiographic data. In the 10 patients in which the gradient was determined, it was found to be above 40 mm Hg in seven cases; three surgical patients had a gradient below 40mmHg. In 2 patients there were calcifications visible in the radiologic exam, with symptoms of syncope and chest pain in another.
The correlation between the surgical findings and the pressure data showed that stenosis was important in the 7 cases with high gradient and mild in the other 3, although there were tense calcifications in 2 cases.
Subsequently, the symptoms of these two cases were related to coronary insufficiency in one case, and to a neurological condition in the other.
Of the 24 patients indicated by clinical data, without determining the gradient, we found symptoms in 13. Mean age in this group was 31 years, with limits of 13-45 years. Eleven of these cases had significant electrocardiographies and 10 had an enlarged cardiac area between + +and+ + +. During the operation, 9 cases had significant stenosis, and in 3, the stenosis was moderate. Eleven cases had no symptoms. The average age of this group was 13 years, with limits of 2-25 years. Only one patient showed severe alterations in the electrocardiogram and 4 had cardiac area between + +and+ + +. During surgery, we found significant stenosis in 3 and moderate in 8 cases.
Surgical treatment consisted of: commissurotomy plus calcium resection in 8 cases, commissurotomy, resection of calcium and a partial prosthesis in one case; resection of calcium and valves plus implantation of a plastic valve in one case, resection of calcium in 1; commissurotomy only, in 11 cases; commissurotomy plus infundibular resection in 3 cases; commissurotomy and resection of the infundibulum plus partial prosthesis; resection of the infundibulum in 6 cases; exploitative aortotomy, not having been identified muscular stenosis in 1 case.
The technique of cardiac arrest during the surgical procedure was performed by anoxia in 2 patients, and by selective hypothermia of the myocardium in 32 others. In 20 of these patients, hypothermia was performed by selective perfusion of cold blood in the aortic root, trying to lower the temperature to 16ºC, which was not always achieved.
In 12 patients, selective hypothermia was performed by using "amorphous ice" in the pericardial cavity; the temperature in these cases was always below 8ºC. The recovery of the heart was not obtained in only one patient in which hypothermia by coronary perfusion was unsatisfactory, above 22ºC, and the perfusion time was long. In another patient, in which selective hypothermia was not satisfactory, the recovery was extremely difficult, taking place in the period post-perfusion, ventricular fibrillation, recovery extremely difficult and time consuming, leading to kidney and brain lesions, with death in the 4
th day.
In the immediate postoperative period, beyond the two deaths mentioned, we had one more in a patient with subvalvular stenosis, which occurred in the second day, with symptoms of severe arrhythmia, with conduction disturbance, probably produced by drugs. The operative mortality in this group was therefore 8.82%.
Among the 31 patients who survived, one death occurred in the 4
th month after surgery. It was a patient of 42 years with fully calcified bicuspid valve. Implantation of two plastic leaflets of Hufnagel was carried out. In the 3rd month of evolution, there was a great decrease in heart size and an accentuated improvement in clinical, electro and vectorcardiographic outcomes. We learned one patient had died suddenly in his hometown in conditions that did not allow us any explanation. Twenty-six patients are well and asymptomatic. In all, there was reduction in heart size and improvement of the electro-and vectorcardiographic outcomes. Three patients had a fair result. Two patients, already mentioned before, had their symptoms resulting from other factors and valvular stenosis, although with a large amount of calcium, it was discreet. The other patient, 46 years and with subvalvular stenosis, had done well over five months and again presented symptoms; he was recatheterized and presented gradient of 60 mm Hg. He is under evaluation, in order to assess the possibility of reoperation. One patient remained unchanged; the muscular stenosis was not recognized during surgery.
The 3 patients operated for aortic insufficiency had a lesion of rheumatic type, with retraction and deformity of the leaflets. All had symptoms, increased heart area and major changes in electro-and vectorcardiographic changes: the diastolic pressure, taken in the arm, amounted to zero in the three cases. The hemodynamic study confirmed major aortic insufficiency in all 3 patients. Cardiac arrest was always made with selective hypothermia, by "amorphous ice" in the pericardium, and lasted for 120, 75 and 70 minutes respectively. The recovery of the heartbeats was possible in all 3 cases, and in all it was implanted an aortic valve of Hufnagel.
Postoperatively, all progressed well. The current follow-up made after 5, 4 and 2.5 months, respectively, shows absence of symptoms, all patients are working, normalization of blood pressure and very accentuated reduction in heart area in two of them and a moderate reduction in one. We have not found yet, electro and vectorcardiographic changes comparable to those observed in radiological imaging.
STUDY OF MAJOR CAUSES OF DEATH WITH THE EMPLOYMENT OF CARDIOPULMONARY BYPASS IN CARDIAC SURGERY. ANALYSIS OF 1668 OPERATIONS PERFORMED IN BRAZIL.
JESSE TEIXEIRA
For this study were requested statistic data to most Brazilian surgeons who practice cardiac surgery with cardiopulmonary bypass, gathering reports on 1668 operations carried out throughout the country until April 1963.
The sources of the investigation are distributed as follows: E. J. Zerbini, São Paulo, 1,000 cases; H. Felipozzi, São Paulo, 377 cases; D. J. Morais, Rio de Janeiro, 147 cases; C. Nogueira, Porto Alegre, 63 cases; L. Tavares da Silva, Recife, 47 cases; M. A. Andrade, Rio de Janeiro, 16 cases; adding 18 additional cases that we operated. Recorded in the entire series, 223 deaths, which amounts to overall mortality of 13.3%.
Having been heterogeneous in their formulation, the causes of death noted by several informants, it seemed necessary to present them sorted into a classification based on analysis of the material received. Operative deaths were divided into four main groups, according to their attribution to circulatory and respiratory causes, the inadequate perfusions and technical failures, the irreversible brain damage and, finally, the unclear causes.
We are the first ones to recognize the artificiality of the causes of death insulation in open heart surgery, because each individual group cannot evade the influence of multiple and complex mechanisms, which were classified under other headings. The admonition is needed to justify the reference to causal factors that, for exhibition purposes, were placed in different categories of what is being analyzed.
I. RESPIRATORY AND CIRCULATORY CAUSES - represent the largest group (116 cases 52% of all surgical deaths), which is understandable when dealing with corrections in the central organ of circulation, to which the lungs are closely linked. Including in this group the failures of the cardiologic sphere: poor selection of cases and misdiagnosis. We can, in principle, obtain favorable results in cardiac surgery under direct vision, to the extent that patients receive the benefit of curative operations, the mortality is always greater when the operations have a purely exploitative nature, the myocardial reserve is scarce, changes in the pulmonary circulation are irreversible and correction of anatomic defect is incomplete or of palliative intent.
The cases that predominate here are of non-operable lesions, but subject to misunderstanding by cardiotomy (Eisenmenger complex, Taussig-Bing anomaly of single ventricle, tricuspid atresia, total form of common atrioventricular channel, tetralogy of Fallot with pulmonary atresia), or of prohibitive surgical risk (ventricular septal defect hypertension, valvular heart disease, acquired with myocardial ischemia or with severe pulmonary disorders). The discrimination of the 116 deaths is as follows:
1.
Cardiocirculatory failure (unspecified) - Under that name we gathered several terminal pathophysiological disorders, whose common feature was the failure of blood circulation, both central and peripheral. There was no means to specify the essence of these disorders because they were labeled generically as "heart failure", "congestive heart failure," "left" or "right" failure, "lack of effective heart beat", "inability to maintain blood pressure", "irreversible shock". Fifty-nine patients died because of this, i.e., 515 in Group I and 26.5% of all the material.
The most common cause of shock after perfusion is heart failure, especially when surgical correction is imperfect or absent, the functional capacity of the myocardium is reduced or the operation is arduous and prolonged; the surgical stress increases the metabolic needs of the body, contributing to harm the recovery of the heart particularly inferior due to the primary lesion and the direct surgical trauma. In a perfect vicious circle, the fall in cardiac output is responsible for poor peripheral circulation (arterial hypotension), with hypoxia textrina, where severe metabolic acidosis, which enhances the final cardiovascular collapse.
Still deserve to be highlighted the following factors of cardiovascular failure: inadequate perfusion, elective misguided cardiac arrest, the ventriculotomy incision, coronary output, preoperative heart failure, cardiac arrhythmias, unnoticed cardiac tamponade , persistent pulmonary hypertension.
2.
Cardiac arrest - A sudden cessation of effective heart beat in diastole or ventricular fibrillation, it was mentioned specifically as a cause of death in 17 cases, representing 14% of Group I and 7.5% of all material. The main factors responsible have been highlighted in the preceding item and should be emphasized; however, the role of the lack of adequate protection to the myocardium during induced assistoles, the common denominator is the myocardial anoxia by insufficient coronary perfusion.
3.
Disorders of the conduction system - Cardiac arrhythmias, especially atrioventricular total block, were the cause of eight deaths (7% of Group I and 3.5% of all the material). Among the most important factors of complication is the vulnerability of the conduction system during the suturing of the septal defect (VSD, tetralogy of Fallot, atrioventricular channel), however, the blocking can occur regardless of direct aggression of the His bundle in patients with severe preoperative myocardial alterations (ASD hypertension) and in the prolonged elective arrests with inadequate myocardial protection. Still, we have marked as lethal arrhythmias, 2 cases of paroxysmal ventricular tachycardia and 2 others not specified, but attributed to the use of chloroform as an anesthetic agent.
4 -
Respiratory failure - Set when the alveolar gas exchanges leave of the usual process, manifesting by hypoxia and hypercapnia. In this series, it was a major cause of death: 24 cases, representing 20.6% of Group I and 11% of all material. It appears when: 1) the thoracic bellows does not guarantee adequate pulmonary ventilation (depression of the respiratory center by anesthetic drugs, insicional pain, reduced cardiac output causing fatigue of the respiratory muscles due to poor perfusion and hypoxia), 2) the functional capacity of the lungs is affected (bronchial secretions accumulus, obstructive atelectasis, bronchial spasm, pulmonary collapse by endothoracic strokes or large cardiomegaly, congestion or acute inflammation of parenchyma, decreased compliance in the mitral rigid lungs).
Specifically related to cardiopulmonary bypass, it should be mentioned the following factors in lung injury: a) interstitial hemorrhage resulting from the sudden increase in left atrial pressure (responsible for numerous deaths in the initial stage of the pioneering experience of surgeons from Sao Paulo, when they were not aware of the need for decompressing the left heart during bypass b) instersticial deposition of hemolysated blood, reducing the alveolocapillary diffusion c) increased alveolar surface tension in very prolonged perfusions, leading to parallel increases in airflow resistance and congestive atelectasis.
5.
Cardiorespiratory failure - There have been eight deaths in which it was not possible to separate the circulatory factor from the respiratory factor (7% of group 1 and 3.5% of all the material). Such morbid association has to be more frequent than one can imagine, being the intimate physiological connections between the heart and lungs. Artificial respiration should, therefore, be maintained for the necessary time in order to recover the hemodynamic and metabolic balance of the patient.
II. INADEQUATE PERFUSION AND TECHNICAL FAILURES - We list herein all deaths directly attributed to imperfections and accidents occurring in perfusion or surgical techniques: 61 cases, totaling 27.5% of all material. That number accounts for the first patients operated by the informants, in the early harsh stage of technical learning and training of teams.
Recently, it has been implicated as a cause of death on cardiopulmonary bypass, biophysical factors, somewhat intangible, such as the denaturation of plasma proteins, causing fat embolism, hemagglutination at the level of arterioles, capillaries and venules, with microinfarctations of vital organs. Such studies seem to come in support of modern techniques of hemodilution and hypothermia, in order to reduce damage during blood perfusion. However, the risk of open-heart surgery depends more on the severity of the lesion to correct than the use of cardiopulmonary bypass.
1.
Metabolic acidosis - Inadequate perfusion with deficit in tissue oxygenation is responsible for a serious state of acidosis, caused by the accumulation of fixed acids (insufficient flow, hypotension, arterial insaturation, severe hemolysis, extended bypass).
It was the cause of death in 22 patients (36% in group II and 10% of all the material).
The difficulties of maintaining proper perfusion are greater in small children (younger than 2 years) and in cases of high hemorrhage through excessive bronchial circulation (tetralogy of Fallot), functioning the latter as ignored
ductus arteriosus or aortic insufficiency.
2.
Acute renal failure - Caused the death of 18 patients (29% of group II and 8% of all the material), the main factor of the complication is the reduction of renal perfusion by low cardiac output and blood pressure. Contributing factors are excessive hemolysis, renal function previously compromised and the administration of incompatible blood. There was a higher incidence of anuria in tetralogy of Fallot
3.
Infection - Death came as a result of infection in 10 patients (16.5% of Group II and 4.5% of all the material); it manifested in the form of bacterial endocarditis, septicemia, suppurative chest or lung disease, occurring lethal results always after the 7
th day postoperatively.
4.
Bleeding - The uncontrollable bleeding was the cause of eight deaths (13% of group II and 3.5% of all the material). Always resulted from technical failures and not of haemorrhagic diathesis: imperfections in vein canullations (1 case) and arterial canullations (2 cases of dissecting aneurysm of the aorta and femoral), cardiorraphy and hemostasis in general.
5.
Recurrence of the defect - Recurrence of ventricular septal defect, for technical failure in the suture of the defect resulted in the deaths of three patients (5% in group II and 1.5% of all the material). Its main cause is the application of surface points for fear of prejudicing the bundle of His.
III. Irreversible brain damage - Thirty-seven patients did not recover consciousness after the perfusion or went into a coma without remission in the immediate postoperative period, representing 16.5% of all material.
Twenty patients had cerebral embolism (54% of group III and 8.9% of all the material), which can be caused by gas (opening of the left heart, low-level of the oxygenator or bubbles formed in the circuit), calcium (mitral and aortic lesions), thrombus (intracardiac clots), fibrin (inadequate doses of anticoagulant) and foreign bodies (silicone). The remaining 17 cases (46% of group III and 7.6% of all the material) were labeled simply as "irreversible brain damage."
The non-embolic cerebral damage occurs due to anoxia of the central nervous system, either by deficient perfusion, circulatory obstruction, prolonged venous hypotension within the superior cava or deep hypothermia.
IV - UNDETERMINED CAUSES - In 9 patients, or 4% of cases, it was not clarified the cause of death.
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license