ABSTRACT
OBJECTIVE: The post operative pain after open heart surgeries had been often reported. Meager reports about respiratory function and pain correlation had been reported. The aim of this article is to assess the pain intensity and location during hospital admittance and its effect on pulmonary function in patients underwent elective cardiac surgery. METHODS: Pulmonary function (lung volumes, respiratory pressures and peak expiratory flow) was assessed at the preoperative and post-operative time (1, 3 and 5 days) by ventilometer, manovacuometer and peak flow meter measurements. The assessment of pain intensity was carried out with a visual analogue scale for pain. RESULTS: The majority of pain site was on sternotomy incision (50% of patients) and the intensity was higher at the first postoperative day (8.32 by visual scale measurement). All pulmonary variables decreased on post-operative time when compared to baseline values. All respiratory variables remained lower than to pre-operative time at fifth postoperative time (P > 0.05), with exception for respiratory rate. The pain and maximal inspiratory pressure showed a negative correlation at the first postoperative day (P = 0.019). CONCLUSION: Postoperative pain decreased lung function in patients precluding deep inspirations, in special, at the first post-operative day.
RESUMO
OBJETIVO: A dor no pós-operatório de cirurgia cardíaca é frequente. Poucos relatos existem sobre a sua relação com a função respiratória e o local mais frequentemente relatado. O objetivo é avaliar a intensidade e a localização da dor durante o período de internação e suas repercussões na função respiratória de pacientes submetidos à cirurgia cardíaca eletiva. MÉTODOS: A função respiratória (volumes pulmonares, força muscular respiratória e pico de fluxo expiratório) foi avaliada nos períodos pré-operatório e pós-operatório (1º, 3º e 5º dia), utilizando os equipamentos ventilômetro, manovacuômetro e medidor de pico de fluxo expiratório. Para mensuração da dor utilizamos a escala visual analógica de dor. RESULTADOS: O local com maior frequência de dor referida foi o esterno (50% dos pacientes) e sua intensidade foi maior no primeiro dia de pós-operatório (8,32 na escala visual analógica). Em todas as variáveis analisadas houve piora dos valores em relação aos obtidos no pré-operatório (P < 0,05) e não observamos o retorno aos valores pré-operatórios até o quinto dia de pós-operatório em todas as variáveis observadas, com exceção da frequência respiratória. Foi observada correlação negativa entre a dor e a pressão inspiratória máxima no primeiro dia de pós-operatório (P = 0,019). CONCLUSÃO: A dor pós-operatória diminuiu a função respiratória nos pacientes avaliados, prejudicando a realização de inspirações profundas, principalmente no primeiro dia de pós-operatório.
INTRODUCTION
In heart surgery, the use of anesthetics and narcotic drugs and the interruption of ventilation in the intraoperative during cardiopulmonary bypass (CPB) associated with pain in the postoperative period leads to decreased ciliary function and limitation of inspiratory effort and impaired effectiveness of cough. This respiratory function deteriorates, predisposing to pulmonary complications [1], such as atelectasis, by hypoventilation secondary to the breathing with low tidal volume caused by pain [2].
Although heart surgery is one of the most extensively studied procedures, the pain in the postoperative (PO) period remains a challenge and needs to be further studied [1,2]. The patient in the PO needs to be mobilized, encouraged to cough to prevent respiratory tract infections and all these activities can be affected by the presence of pain. The measurement of pain is helpful to recognize the amount of pain perceived by the patient and to compare with other painful experiences [1].
The pain has been reported as the first complaint of patients in heart surgery PO and intensive care units [3]. There are few reports on the relationship of the PO pain and changes in respiratory dynamics [1,3-5].
Therefore, the capital aim of this study was to assess the location and intensity of pain reported by patients undergone heart surgery and to assess the correlation between pain and changes in variables that analyze the respiratory function.
METHODS
After approval by the ethics committee of the institution, under number 145/2007, patients undergoing heart surgery via median sternotomy with CPB (CABG, valve replacement or both) were included in the study randomly, according to the sequence of surgeries performed from August to December 2007.
Patients were approached in the preoperative period for questions and obtaining writen informed consent, demographic data collection and evaluation of lung function.
Initially, 36 patients were selected to participate in the study and some of them were excluded for the following reasons: personal refusal during the protocol (two patients), hemodynamic instability in the postoperative period (two patients) and reoperation (one patient).
All patients underwent general venous and balanced inhalational anesthesia with use of midazolam (0.05 mg/kg), sufentanil (1-2mcg/kg), pancuronium (0.1 mg/kg) and isoflurane (0.5-1%).
Heart surgery was performed via longitudinal median sternotomy using CPB with arterial cannulation of the ascending aorta and single atrial venous cannulation. At the end of the procedure it was performed drainage using negative suction drain of 6.4 mm in diameter in the pericardium and retrosternal tubular drain number 36 with water seal, maintained in aspiration with 20 cm of water. These drains were removed 48 hours after surgery.
In the postoperative period, analgesia was performed in accordance with the request of the patient, based on dipyrone intravenously and intravenous morphine without anti-inflammatory drugs associated.
Patients were extubated in the postoperative period after reaching the Ramsay scale = 2, that is, being without sedation, intermittent or continuous, cooperative, oriented and tranquil, but with analgesia according to the protocol of analgesia, hemodynamic stability, presenting index of rapid superficial breathing under 100 and maximum inspiratory pressure (MIP) over-25cmH
2O [6]. All patients received physiotherapy in the postoperative period, according to the service routine.
The measures of lung volumes were performed with the spirometer (FERRARIS Wright ® MK 8) coupled to a nozzle. The patient was guided to breathe quietly in the apparatus for a minute for reading of the minute volume (VM). During this period, it was found the number of breaths, that is, respiratory frequency (RF) to calculate the current volume (CV) given by the formula CV=MV/RF (ml) [7].
The peak expiratory flow was obtained using the equipment Peak Flow (ASSESS ®). The patient was guided to perform a maximal inspiration up to total lung capacity, followed by an inspiratory pause of at most two seconds, and to perform a forced expiration. Three measurements were performed with an interval of 30 seconds, by accepting 10% variability between them, with the largest value considered valid [8].
The inspiratory muscle strength was measured by the manovacuometer (Gerar ®) coupled to a mouthpiece and nose clip, determining maximum inspiratory pressure (MIP) and maximal expiratory pressure (MEP). The patient was positioned lying on the bed at a 45-degree angle.
To measure the MIP it was requested a maximal expiration up to residual volume, followed by a maximal inspiratory effort sustained for about one second, with occlusion of the manovacuometer done manually. The maneuvers were repeated three times at intervals of one minute, and it was considered the largest measure obtained. The last maneuver should not be the largest of the series and the variability between the best two readings should not exceed 10% of the second largest measure.
To measure the MEP was used the same technique used to verify the MIP, but it was requested a maximal inspiratory effort to achieve the level of total lung capacity and the reading was taken after the occlusion of the mouthpiece and a maximum expiratory effort of the patient [9].
The perception of pain was obtained using a visual analogic pain scale of zero to ten [10]. All data were collected preoperatively (PrO), 1
st PO, 3
rd PO and 5
th PO.
Numerical variables were expressed as mean and standard deviation and categorical variables as frequency. The Kolmogorov-Smirnov test was used to verify the normal distribution of variables; it was used the Spearman correlation test for univariate analysis between pain and respiratory variables, and the Friedman test was used to analyze continuous variables for serial measurements. The chi-square test was used to describe the location of the pain reported by patients. The value of
P < 0.05 was considered statistically significant.
RESULTS
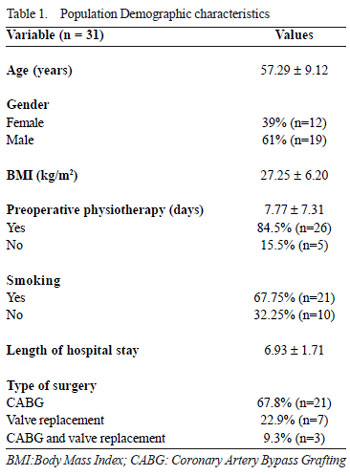
The sample consisted of 31 patients aged 57.29 ± 9.12 years with male predominance (61%). The demographic characteristics of patients are shown in Table 1. Patients who underwent reoperation were not inclucled.
It was observed that the variables used to evaluate respiratory function - minute volume, tidal volume, peak expiratory flow, maximal inspiratory and expiratory pressures - were lower when compared to preoperative period (
P < 0.01). This difference was maintained during the postoperative period of follow-up of this study.
The perception of pain was greater in the postoperative period (
P < 0.01), with its greater value in the 1
st PO. Data are summarized in Table 2.
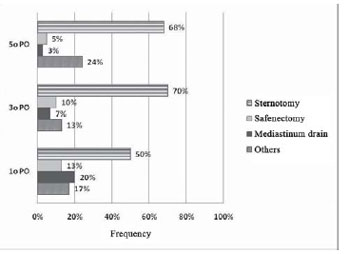
The most frequently reported site pain was the median sternotomy in all periods studied (
P = 0.002) (Figure 1).
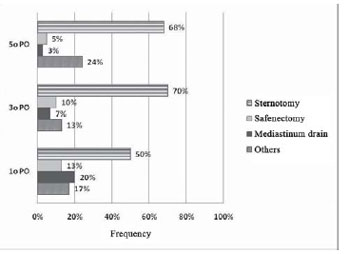
Fig. 1 - Distribution of pain in the postoperative period. 1
st PO = first postoperative day, 3
rd PO = third postoperative day, 5
th PO = fifth postoperative day
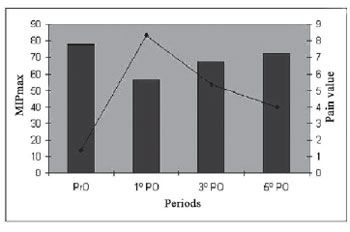
There was correlation of pain in the 1
st PO with the decrease in MIP (
P < 0.001), and there were no other correlations in other variables (Figure 2).
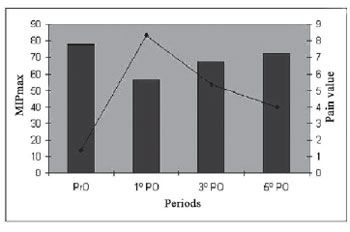
Fig. 2 - Correlation between MIP and pain referred in the sternotomy at moments PrO, 1
st PO, 3
rd PO and 5
th PO). (*) P < 0.019. - Legend: 1
st PO = first postoperative day, 3
rd PO = third postoperative day, 5
th PO = fifth postoperative day
Pain in the postoperative period of heart surgery is a common sense, and can interfere with lung function, increasing the incidence of morbidity and mortality in this period. The pain reported in this study was present at all times assessed, especially in the 1
st PO. The worsening of pain has shown positive correlation with the worsening of lung function, which was observed until the 5
th PO. The parameters of respiratory function did not return to the values observed in the preoperative period.
We observed that the average of the pain referred preoperatively was 1.38, being more intense in the 1
st PO, and decreasing in the 3
rd and 5
th PO. We also observed correlation of pain with worsening of MIP on the 1
st PO and the principal location of pain sense was median sternotomy.
Some series reported pain equal to zero or with values close to it by the visual analog scale in the preoperative period [11,12]. In our series we observed value of 1.38, which can be attributed to the presence of angina or anxiety in the preoperative period, because most of the population had coronary artery obstruction and had undergone coronary artery bypass grafting [13,14].
Pain in the postoperative period was more intense in the 1st PO, decreasing gradually in the 3
rd and 5
th PO, which is also reported in other experiences with the greatest intensity of pain in the 1
st and 2
nd PO [5.15]. The protocols of postoperative analgesia vary between institutions, however, we can not affirm that these findings or even compare them.
Other series have reported that increased pain may occur after the first week of surgery and with significant complications on pulmonary function [5]. This can be explained by inadequate pain control after discharge from hospital. In our study, the observation was performed only during the hospital stay, with no observation periods longer than five days.
The prevalent location of pain reported in this study was the sternotomy. Although the impact of median sternotomy in pulmonary dysfunction postoperatively is not well understood, studies report its relationship to changes in respiratory function, leading to shallow breathing, impaired in gas exchange and susceptibility to pulmonary complications in the postoperative [16]. It was observed by some authors that the number of locations with pain does not vary with time, but rather its location [5]. In our report we did not observe this location migration of the referred pain.
We could demonstrate that the worsening of pain led to significant worsening of the MIP in the 1
st PO, which is not completely restored until the 5
th PO, however, in this study the pain was not significantly associated with patient's characteristics and with the surgical procedure.
Cipriano et al. [17] and this study found significant decrease in lung volumes between the pre- and postoperative periods with correlation with pain with this variable in the postoperative period.
Some authors found no decrease in MIP in the postoperative period and reported that the effective action of physiotherapy provided these results [12].
In our study the location of the median sternotomy was the most often associated with the referred pain. This finding, to our knowledge, is not often reported in the literature. Mueller et al. [3] reported that pain related to nocireceptive stimuli as drains and endotracheal tube disappear after the 3
rd PO. However, pain of osteoarticular origin, due to the opening of the chest cavity, becomes more evident after this period [3].
The presence of the pleural drain is also an important cause of postoperative pain. Guizilini et al. [18] reported that coronary artery bypass grafting without cardiopulmonary bypass, irrespective of the drain location, causes pain and significant drop in lung function and its insertion in the subxiphoid region showed less subjective pain and a better preservation of pulmonary function when compared to the intercostal insertion. In this study, the insertion of the drain was always performed in the subxiphoid region and removed on the 2
nd PO as routine. The length of stay of the drain is also important in the degree and location of the referred pain, and patients with shorter duration of chest drain present less pain and less migration of it [3].
Previous studies have shown that, irrespective of surgical technique used, CPB causes lung damage and delayed recovery of lung function [17]. Other authors studied lung function in patients undergoing surgery with ou without CPB and identified a better pulmonary function in the group who underwent cardiac surgery without CPB [19].
In our study, we did not evaluate gas exchange. Literature reports describe the decrease in relationship between arterial oxygen pressure and inspired oxygen fraction (PaO
2/FiO
2) during the perioperative period [20].
The alveolar hypoventilation due to pain in the sternotomy location is a common cause of atelectasis in the postoperative period [21,22]. The use of anesthetics and the absence of alveolar ventilation during CPB cause decreased ciliary function. The pain and the effectiveness of the cough reflex are also impaired during this period.
Other studies showed that several physiotherapeutic strategies do not prevent the decrease of MIP and MEP [21]. Romanini et al. [23] demonstrated that MIP and MEP have shown a significant decrease between preoperative and postoperative periods and the 1
st PO day in the group treated with positive pressure in the airways and in the group undergoing conventional physiotherapy.
Cough is a very painful activity after open heart surgery, which may favor the retention of secretions in the airways, an important risk factor for postoperative pulmonary complications [24,25].
In a recent study, Tonella et al. [26], using transcutaneous electrical stimulation have shown pain relief in postoperative abdominal surgery, on which the patients in the study group had lower pain scores during forced coughing and respiratory incentives. This type of therapy may also be used for patients in the postoperative of heart surgery with the benefit of reduced use of sedatives and their side effects.
The limitations of our study are the inclusion of radiological examinations, which could show pulmonary complications of different proportions, affecting the values of lung function. All pulmonary function tests depend on specific maneuvers and the patient's will to perform them. The group has small number of patients, however, we could demonstrate the relationship between pain and reduced respiratory function.
CONCLUSION
Our findings demonstrate that pain is present even before the surgery and is important in respiratory function in the postoperative period. The most common location was the median sternotomy, which may worse bronchial hygiene.
These findings lead us to develop different strategies in the treatment of pain and physiotherapy that may interfere with pain, with consequent improvement in pulmonary function.
REFERENCES
1. Arcêncio L, Souza MD, Bortolin BS, Fernandes ACM, Rodrigues AJ, Évora PRB. Cuidados pré e pós-operatórios em cirurgia cardiotorácica: uma abordagem fisioterapêutica. Rev Bras Cir Cardiovasc. 2008;23(3):400-10. [MedLine] View article
2. Schuller D, Morrow LE. Pulmonary complications after coronary revascularization. Curr Opin Cardiol. 2000;15(5):309-15. [MedLine]
3. Mueller XM, Tinguely F, Tevaearai HT, Ravussin P, Stumpe F, von Segesser LK. Impact of duration of chest tube drainage on pain after cardiac surgery. Eur J Cardiothorac Surg. 2000;18(5):570-4. [MedLine]
4. Brasil LA, Gomes WJ, Salomão R, Buffolo E. Inflammatory response after myocardial revascularization with or without cardiopulmonary bypass. Ann Thorac Surg. 1998;66(1):56-9. [MedLine]
5. Mueller XM, Tinguely F, Tevaearai HT, Revelly JP, Chioléro R, von Segesser LK. Pain location, distribution, and intensity after cardiac surgery. Chest. 2000;118(2):391-6. [MedLine]
6. Goldwasser R, Farias A, Freitas EE, Saddy F, Amado V, Okamoto V. III Consenso Brasileiro de Ventilação Mecânica: Desmame e interrupção da ventilação mecânica. Sociedade Brasileira de Pneumologia e Tisiologia. J Bras Pneumol. 2007;33(Supl. 2):S128-36. [MedLine]
7. Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. 1991;324(21):1445-50. [MedLine]
8. Miller MR, Dickinson SA, Hitchings DJ. The accuracy of portable peak flow meters. Thorax. 1992;47(11):904-9. [MedLine]
9. Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969;99(5):696-702. [MedLine]
10. Gift AG. Visual analogue scales: measurement of subjective phenomena. Nurs Res. 1989;38(5):286-8. [MedLine]
11. Borges JBC, Ferreira DLMP, Carvalho SMR, Martins AS, Andrade RR, Silva MAM. Avaliação da intensidade de dor e da funcionalidade no pós-operatório de cirurgia cardíaca. Rev Bras Cir Cardiovasc. 2006;21(4):393-402.
12. Leguisamo CP, Freitas MF, Maciel NF, Donato P. Avaliação da dor e da função pulmonar em pacientes submetidos à cirurgia de revascularização miocárdica. Fisioter Bras. 2007;8(1):14-8.
13. Markou AL, van der Windt A, van Swieten HA, Noyez L. Changes in quality of life, physical activity, and symptomatic status one year after myocardial revascularization for stable angina. Eur J Cardiothorac Surg. 2008;34(5):1009-15. [MedLine]
14. Greszta E, Sieminska MJ. Relationship of preoperative anxietystate and anxiety-trait in patients qualified for coronary artery bypass graft surgery to the perception of postoperative pain and other pain complaints. Ann Acad Med Stetin. 2008;54(1):157-63. [MedLine]
15. Giacomkazzi CM, Lagni VB, Monteiro MB. A dor pósoperatória como contribuinte do prejuízo na função pulmonar em pacientes submetidos à cirurgia cardíaca. Rev Bras Cir Cardiovasc. 2006;21(4):386-92.
16. Wynne R, Botti M. Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care. 2004;13(5):384-93. [MedLine]
17. Cipriano G Jr, Camargo Carvalho AC, Bernardelli GF, Tayar Peres PA. Short-term transcutaneous electrical nerve stimulation after cardiac surgery: effect on pain, pulmonary function and electrical muscle activity. Interact Cardiovasc Thorac Surg. 2008;7(4):539-43. [MedLine]
18. Guizilini S, Gomes WJ, Faresin SM, Carvalho ACC, Jaramillo JI, Alves FA, et al. Efeitos do local de inserção do dreno pleural na função pulmonar no pós-operatório de cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2004;19(1):47-54. View article
19. Ng CS, Wan S, Yim AP, Arifi AA. Pulmonary dysfunction after cardiac surgery. Chest. 2002;121(4):1269-77. [MedLine]
20. Barbosa RAG, Carmona MJC. Avaliação da função pulmonar em pacientes submetidos à cirurgia cardíaca com circulação extracorpórea. Rev Bras Anestesiol. 2002; 52(6):689-99. [MedLine]
21. Silva NLS, Piotto RF, Barboza MAI, Croti UA, Braile DM. Inalação de solução salina hipertônica como coadjuvante da fisioterapia respiratória para reversão de atelectasia no pósoperatório de cirurgia cardíaca pediátrica. Rev Bras Cir Cardiovasc. 2006;21(4):468-71.
22. Magnusson L, Zemgulis V, Wicky S, Tydén H, Thelin S, Hedenstierna G. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass: an experimental study. Anesthesiology. 1997;87(5):1153-63. [MedLine]
23. Romanini W, Muller AP, Carvalho KAT, Olandoski M, Faria-Neto JR, Mendes FL, et al. Os efeitos da pressão positiva intermitente e do incentivador respiratório no pós-operatório de revascularização miocárdica. Arq Bras Cardiol. 2007;89(2):105-10.
24. Milgrom LB, Brooks JA, Qi R, Bunnell K, Wuestfeld S, Beckman D. Pain levels experienced with activities after cardiac surgery. Am J Crit Care. 2004;13(2):116-25. [MedLine]
25. Fiore JF Jr, Chiavegato LD, Denehy L, Paisani DM, Faresin SM. Do directed cough maneuvers improve cough effectiveness in the early period after open heart surgery? Effect of thoracic support and maximal inspiration on cough peak expiratory flow, cough expiratory volume, and thoracic pain. Respir Care. 2008;53(8):1027-34. [MedLine]
26. Tonella RM, Araújo S, Silva AMO. Estimulação elétrica nervosa transcutânea no alívio da dor pós-operatória relacionada com procedimentos fisioterapêuticos em pacientes submetidos a intervenções cirúrgicas abdominais. Rev Bras Anestesiol. 2006;56(6):630-42. [MedLine]
Article receive on Monday, June 1, 2009
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license