OBJECTIVE: To present the Instituto de Cirurgia Cardiovascular do Oeste do Paraná' (ICCOP) surgical experience, on the treatment of left ventricle aneurysms, by endoventriculoplasty, with septal exclusion (EVSE), and a 111 months follow-up. METHODS: Between April 1999 and April 2006, 28 patients were submitted to EVSE, by the author. Pre, trans and late post clinical and echocardiographic variables were analyzed retrospectively. Mean age was 59.0 ± 9.5 years, being 23 male patients. Seventeen patients were in NYHA functional class IV and the mean EuroScore was 8.2 ± 2.3. The mean pre-operative values for ejection fraction, end systolic and diastolic left ventricular volumes were 32.3 ± 9.2%, 113.9 ± 36.0 ml e 179.2 ± 48.4 ml, respectively. The BraziliAnVErsion of the SF36 quality of life questionnaire was applied in the late follow up period. RESULTS: Four patients died in the immediate post-operative period, being the major cause of morbidity low cardiac output syndrome and arrhythmias. The mean follow-up period was 5.6 ± 3.2 years. Left ventricle's ejection fraction and aortic cross clamping time were the significant factors for hospital and late mortality with P = 0.0222 and P = 0.0123, respectively. Actuarial survival curve showed a survival of 82.1 ± 7.2%, and 54.7 ± 22.9%, pre and post 107 months, of follow-up. CONCLUSION: EVSE' surgery is an effective option to treat this group of patients, with improvement of left ventricular function (from 32.3 to 46.4%) and patients' quality of life.
OBJETIVO: Apresentar a experiência do Instituto de Cirurgia Cardiovascular do Oeste do Paraná (ICCOP) com o tratamento de aneurismas de ventrículo esquerdo, com a técnica de endoventriculoplastia com exclusão septal (EVES), imediata e o seguimento por 111 meses. MÉTODOS: No período de abril de 1999 a 2006, 28 pacientes foram submetidos a EVES, pelo autor. Foram analisadas, retrospectivamente, variáveis clínicas e ecocardiográficas pré, trans e pós-operatórias tardias. A idade média era de 59,0 ± 9,5 anos, sendo 23 pacientes do sexo masculino. Dezessete pacientes estavam em classe funcional IV e o EuroScore médio foi 8,2 ± 2,3. Os valores pré-operatórios de fração de ejeção, volumes sistólico e diastólico finais do ventrículo esquerdo foram, respectivamente, 32,3 ± 9,2%, 113,9 ± 36,0 ml e 179,2 ± 48,4 ml. Foi aplicada a versão brasileira do questionário de qualidade de vida SF36 no pós-operatório tardio. RESULTADOS: A mortalidade imediata foi de quatro pacientes por síndrome de baixo débito e arritmia. O tempo médio de seguimento pós-operatório foi 5,6 ± 3,2 anos. A fração de ejeção de ventrículo esquerdo foi fator significativo na mortalidade imediata (P=0,0222) e o tempo de parada cardíaca anóxica na tardia (P=0,0123). A análise atuarial de sobrevivência demonstrou uma sobrevida de 82,1 ± 7,2%, e 54,7 ± 22,9%, respectivamente, antes e depois de 107 meses, de seguimento. CONCLUSÕES: A cirurgia da EVES é efetiva no tratamento desse grupo de pacientes, com melhora da função ventricular esquerda (de 32,3 para 46,4%) e da qualidade de vida dos pacientes.
INTRODUCTION
One of the causes of congestive heart failure is left ventricular aneurysm (LVA), post-myocardial infarction, coronary artery disease, and its treatment remains one of the topics on which there is no consensus regarding the surgical technique to be used. Heart failure today is the leading cause of hospital stay in the hospital network, including both national statistics and the international [1,2] and it is a syndrome of difficult treatment, dependent on its etiology and treatment to be accomplished, that in patients with moderate to severe involvement presents low prognosis of survival in five years of evolution.
The LVA presents an incidence of 10% to 30% among cases of myocardial infarction (AMI), although apparently reduced, in view of the effectiveness of both the diagnosis and early treatment of AMI, affects up to 85% of the left ventricular anterolateral wall (LV).
For such patients with dilation and loss of normal left ventricular geometry, one should take into consideration the prevention of future ischemia through coronary revascularization, and reduction of sequels from muscle necrosis in cardiac structures, with preservation of ventricular structure and function, especially with regard to systolic and diastolic left ventricular dysfunctions. For these factors are met, there is a need to correct the remodeling that occurs after infarction, with the progressive temporal deterioration of cardiac function, by means of reverse remodeling surgery. Some authors demonstrated that, despite improvement in symptoms of angina, patients with low ejection fraction who had undergone only coronary artery bypass grafting, present survival below the expected [3].
Several techniques have been proposed for the treatment of this sequel, which began more than five decades agor, with the studies by Likoff and Bailey, who performed the first left ventricle aneurysmectomy in a beating heart, with lateral clamping and through lateral thoracotomy. With the advent of cardiopulmonary bypass, the treatment was performed with resection of necrotic and/or ischemic tissue [4], represented by akinetic or dyskinetic areas, by ventricular resection surgery, with plication or linear closure, which became the "gold standard" in the following decades. However, with this technique on which the area at risk of being resected is very important in left ventricular function, and on which its resection causes not only decrease of the volume and shape of the remaining ventricular cavity, as well as loss of contractile force and ventricular geometry, there is improvement of the original presentation, but with unsatisfactory mid- and long-term evolution [5].
In 1985, Jatene [6] presented the new concept of geometric reconstruction of the LV, with the restoration of the LV elliptical shape, which the author referred it as the factor of change of the results when analyzed 508 patients undergone surgery between 1977 and 1983. In subsequent studies, Dor et al. [7] presented their initial experience of 25 cases using the concept of Jatene and confirming the results obtained by him. After the initial results, other groups, such as Cooley [8] in 1989, and Mickleborough et al. [9] in 1994, published their results with different techniques.
The main factor of all these techniques, based on the preservation of physiology, as similar as possible to normal, from the preservation of the anatomy of the left ventricle, taking into account that it must repair the elliptical shape, recreating an apex, reducing the mitral annulus, when it is enlarged, and restore the geometry of the papillary muscles. These corrections lead to physiological improvement, depending on the technique of reverse remodeling that also reduces wall tension and improve systolic function.
Our experience started in 1999 [10], when we fond that after the LVA, both the LVA's of large hemodynamic consequences, such as large volume, presented different results when compared to others treated by linear technique [11]. Thus, we began this surgical technique described by Dor in a group of patients in which the clinic more prevalent was heart failure and very severe deformity of the LV, without the use of grafts, except for one case. Other national authors also reported this surgical technique [12].
The main objective of this study is to show the early and late results of the Instituto de Cirurgia Cardiovascular do Oeste do Paraná (ICCOP), in a consecutive series of patients undergoing reconstruction of left ventricular geometry through the technique of endoventricular repair with septal exclusion for correction of aneurysms of the anteroseptal wall of this ventricle, operated by the same surgeon. As a secondary pupose it will be shown: 1) survival curve of these patients, 2) factors contributing to unfavorable surgical outcome, 3) the relationship of clinical status, subjective of patients and its correlation with echocardiographic parameters.
METHODS
From April 1999 to April 2006, 71 patients underwent surgery for treatment of aneurysms of the left ventricle, of ischemic origin with areas with dyskinesia and/or akinesia at Instituto de Cirurgia Cardiovascular do Oeste do Paraná (ICCOP). Of these, 28 (39.4%) underwent surgery to reverse remodeling, according to the technique of circular endoventricular repair, excluding septum, with or without the use of heterologous graft because they present significant increase in left ventricular end-systolic volume (LVESV) and/or left ventricular end-diastolic volume (LVEDV), with ventricular dysfunction and symptoms of heart failure, angina or arrhythmia. In all patients coronary angiographies and/or echocardiography were performed, from where the data reported herein were obtained.
Data were obtained retrospectively through review of medical records and examinations performed preoperatively. The data included: 1) demographics - age, gender, weight, height, body surface, body weight, surgical indication, date of surgery, type of surgery (elective, urgent, emergency, first surgery or reoperation) and surgeon;2) clinical classification of functional class of heart failure, according to the New York Heart Association (NYHA) and surgery classification through the evaluation of surgical risk by EuroSCORE, 3) comorbidities as risk factors - hypertension, chronic obstructive pulmonary disease, diabetes mellitus, stroke and kidney failure, 4) echocardiographic data (performed by observers and using different techniques) - mitral regurgitation, ejection fraction (EF), LVESV and LVEDV, 5) surgical data, such as type of surgery (alone or associated reverse remodeling), associated procedures, time of cardiopulmonary bypass and anoxic cardiac arrest (clamping), use of left ventricular assist devices and intra-operative complications, 6) data of postoperative, complications such as bleeding with surgical indication of exploratory thoracotomy, surgical infections, use of mechanical ventilation over 24 hours, syndrome of low cardiac output and use of left ventricular assist devices.
The long-term follow-up was performed prospectively by direct contact with the patient personally, by phone or with their families, or also contact with his assistant physician. In these, it was applied a modified questionnaire of quality of life SF36, and data (EF, LVESV and LVEDV) of echocardiograms were assessed, performed six months before such assessment. The Research Ethics Committee of the Research and Postgraduation Dean's Office of the State University of Oeste do Paraná approved this research through the 432/2008-CEP approval.
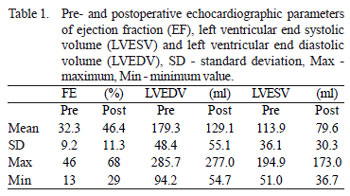
Male were predominant, represented by 23 (82.1%) patients, mean age 59.0 ± 9.5 (57.5 for males and 65.8 for females) and functional class, according to NYHA, of 3.6 ± 0.5, on which 60.7% were in class IV. All aneurysms of this group were antero-apical, always with concomitant involvement of the interventricular septum, diagnosed preoperatively, but in different degrees. The main clinical indication for surgery was heart failure in 20 (71.4%) patients, angina in seven (25.0%) and arrhythmia in one (3.6%). In all patients preoperative echocardiograms were performed for evaluation of ejection fraction by Simpson's method, and calculation of end systolic and diastolic volume of the left ventricle, as shown in Table 1.
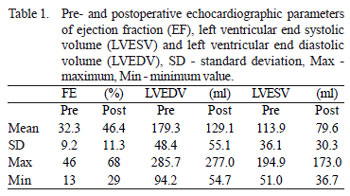
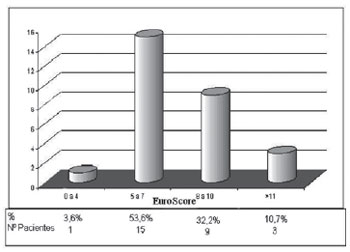
Mitral insufficiency was moderate in two (7.1%) patients, mild in eight (28.6%) and trivial or absent in the remaining patients. The average time between the completion of cineangiocoronariography and surgery was 84.0 ± 67.5 days. The additive EuroSCORE was, on average, 8.2 ± 2.3 and the calculation of logistic regression of 11.5 ± 9.1. Figure 1 shows the distribution of patients in various bands of additive EuroSCORE. Surgery was performed emergently, defined as any surgery performed within 24 hours after admission, but without any prior planning, in only four (14.3%) cases, and the remaining were elective. All procedures were first surgeries.
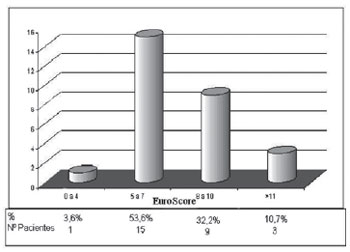
Fig. 1 - Distribution of patients by groups of the additive EuroSCORE
The surgeries were performed under general anesthesia with the use of cardiopulmonary bypass, moderate systemic hypothermia (28°C to 30°C), cold crystalloid cardioplegia and Shumway solution, in all cases, except for one, it was performed protection of the phrenic nerve. The left ventricular cavity was opened after aortic clamping and cardiac aspiration of the proximal aorta, to identify the aneurysmal area, through an incision parallel to the interventricular septum, and anterior interventricular artery. When there was presence of thrombi, they were harvested and cleaning was performed in the LV. In the transition zone between normal muscle and that one presenting fibrosis, a circular suture, tobacco-pouch type, was performed to resize the heart cavity with a 3-0 polypropylene thread. The fibrous portion of the interventricular septum was dissected from the rest, between the apical portion of the LV and the crossing path of the circular suture. This patch was used for closing the left ventricular cavity.
The excess of the aneurysm wall was resected, leaving only what was strictly necessary for closure - jacket suture, thus ensuring perfect hemostasis at the end. After the completion distal anastomoses of grafts were prepared for myocardial revascularization. The proximal anastomoses were performed with partial aortic clamping, except when it was extremely calcified (3.6%), on which were performed with total clamping. The mitral valve was not approached in any of the patients in this group.
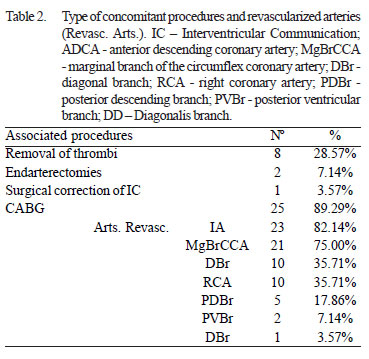
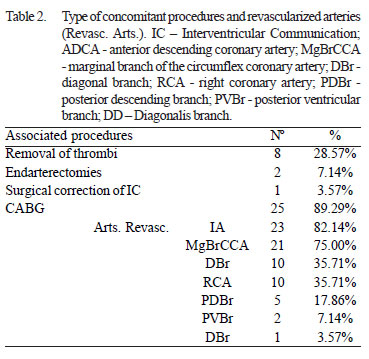
In this group of patients, surgery to reverse remodeling without concomitant coronary artery bypass grafting (CABG) was performed in only three (10.7%) patients, but only in one case the surgery was performed alone. In eight (28.6%) patients there were harvesting of thrombi in the left ventricle, in two (7.1%) coronary endarterectomy and in one case (3.6%) closure of an interventricular communication. In 25 (89.3%) patients undergone CABG, the mean number of grafts was 2.9 (minimum of one and a maximum of five), with 1.96 and 0.92 venous and arterial grafts per patient respectively, and the left internal thoracic artery was used in 92% of procedures. The anterior interventricular artery was the most revascularized, in 82.1% of patients. Table 2 shows the type of concomitant procedures and the revascularized arteries. In only one (3.6%) case a graft of heterologous bovine pericardium was used for correction of LVA.
Ventricular assist devices were used in some cases: placement of intra-aortic balloon (IAB), preoperatively, in four (14.3%) patients; in the intraoperative was performed derivation of the left atrium/aorta in one (3.6 %) case. The average length of stay of the IAB was 26.3 ± 16.9 hours, and the derivation of 83 minutes.
The mean time of cardiopulmonary bypass and anoxic cardiac arrest were respectively 113.9 ± 38.9 (min = 67 and max = 234) and 49.4 ± 13.0 (min = 29 and max = 80) minutes.
Assessments were performed using the Brazilian version of the quality of life questionnaire SF36 [13] of 23 patients, either by direct information or by contact with their families or with the assistant physician in a period not exceeding six months before of the completion of this study. The value for each of the eight areas was calculated and assessed on a scale ranging from 0 to 100, where zero is the worst condition and one hundred is the best.
Statistical analysis was performed by the representation of the data as mean and standard deviation. The variables were analyzed by relative risk (comparison of two linear variables), multiple linear regression (multivariate linear variable analysis) and analysis of Kaplan-Meier (survival curves). The analysis was performed with the StatsDirect Statistical Software. P values below 0.05 were considered significant.
RESULTS
The most frequent complications, in the transoperative syndrome were low cardiac output in five (17.9%), LV bleeding in three (10.7%) and arrhythmia in two (7.1%) patients. The use of inotropic drugs was performed in 33.3% of patients. Mechanical ventilation was maintained for more than 24 hours in only two (7.4%) patients.
The main causes of morbidity in this period were: syndrome of low cardiac output (8), arrhythmia (3), acute renal failure (1), respiratory failure (1) and transient ischemic stroke (1). Eight (33.3%) patients needed to use of catecholamines at high doses. The average hospital stay in the postoperative was 7.4 ± 4.1 days and, if we consider only patients who were discharged from hospital at 7.50 ± 1.7 days, the average time of stay in the intensive care unit (ICU) was 3.3 ± 4.4 (1 to 24) days. Four patients died, corresponding to 14.3% in the trans- or postoperative period. Of these, 75% presented an ejection fraction below 24%. The causes of death were left ventricular failure, intra-operatively in one patient and one on the 2nd postoperative day, arrhythmia syndrome and low cardiac output, on the 2nd postoperative day, pulmonary and neurological complications on the 24th postoperative day.
The mean time of postopeartive follow-up was 5.6 ± 3.2 years (until July 2008). The 24 patients who were discharged from hospital were assessed in the first 30 days, by the surgeon, and after by their cardiologists. Follow-up was obtained in 100% of the survivors. Two patients died during follow-up, the causes of death were left ventricular failure in both cases, at four and 107
th months.
The relative risk between the study group and the EuroSCORE, was 1.75, with an increased relative risk of 0.75 and an absolute of 6.1%. The functional class according to NYHA, of the 23 survivors was 1.5 ± 0.7, and in 60.9% the functional class was I.
Multiple linear regression was performed to assess the variables, age, gender, NYHA functional class, ejection fraction, end systolic and diastolic volumes of LV and times of cardiopulmonary bypass and cardiac arrest, as well as weight, height, body surface and body mass, had influenced the final outcome, mortality, both immediate and during the follow-up period. When the variables were analyzed in relation to immediate mortality, the ejection fraction was statistically significant with a P = 0.0222. Comparing the three variables, with greater tendency to significance, ejection fraction, functional class and time of cardiac arrest, only the first is significant, with P = 0.0125. In relation to overall mortality, when analyzing the time of cardiac arrest, the variable with significance with P = 0.0123 and the three most important variables were gender, time of cardiac arrest and ejection fraction, and the first two statistically significant with P = 0.0068 and P = 0.0049, respectively.
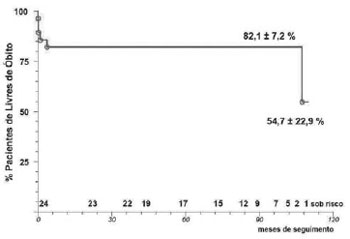
The actuarial analysis of survival by Kaplan-Meier, in patients undergoing geometric reconstruction, showed survival of 82.1 ± 7.2%, 82.1 ± 7.2% and 54.7 ± 22.9%, respectively, at the end of 50, 100 months and 110 months (Figure 2).
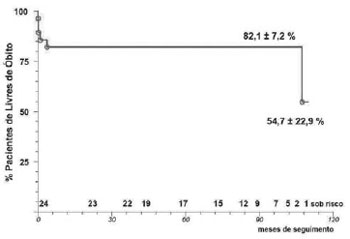
Fig. 2 - Kaplan-Meier survival curve of the endoventricular repair surgery with septal exclusion of 28 patients with 111 months of follow-up
The outcome of 23 patients assessed through the questionnaire of quality of life SF36, in the postoperative period until six months before the end of data collection, has shown quality of life a little better than before surgery (2.4 ± 1.2). In relation to the gross scale, from the eight areas assessed, the pain presented a value of 74, a functional capacity of 65, the general health condition of 52.5, the mental health of 49.2, physical limitations of 46.5, social limitations of 40.1, vitality of 39.3 and limitation by emotional aspects of 54.7.
In the analysis of the values of EF, LVESV and LVEDV, there was improvement, respectively, of 46.4 ± 11.3%, 126.1 ± 55.1 ml and 79.6 ± 30.3 ml, an improvement when compared with the data obtained before surgery with values of 43.7%, 42.2% and 43.1%, respectively.
DISCUSSION
The purpose of the surgery of left ventricular reverse remodeling is to reduce the volume of the left ventricular capacity and restablish its pre-remodeling form, as well as a complete revascularization. When this technique has started, and based on the literature, there was a reality on which in adittion to improve survival of patients with extensive sequelae of myocardial infarction, corresponding to large losses of muscle necrosis of the left ventricle, there would also be improved quality of life of them. This inference was performed when comparing studies with the results of this technique and the studies that analyzed the survival of heart failure that demonstrated improved survival for patients with symptoms of heart failure over the past decades [14], but survival in average at the end of five years is 50%. Patients in this study presented, as main symptom, in 71.4% of them, heart failure, and therefore their evolution can be comparable.
More recent studies [15,16] demonstrate that surgical repair of ventricular geometry improves cardiac parameters and thus the survival of patients with left ventricular remodeling of both ischemic ethiology and patients with dilated cardiomyopathy can be compared.
Previous studies performed in single centers [17,18], and multicenter studies [16] have shown excellent results with this technique, both at mid- and long-term.
The association of coronary artery bypass grafting with the reverse ventricular remodeling is based on studies showing that, although there is viable myocardium after MI, the presence of an increased end-systolic volume, decreases the improvement of global cardiac function [19]. Concerning the previous considerations, the restoration of normal geometry associated with CABG demonstrates not only improvement of the parameters of the left ventricle, but also survival and long-term quality of life.
Although the sample size presented in this study is not ideal to take the conclusions based on statistical significance, some points can be compared and discussed.
When analyzing the postoperative complications [20], it can be found a correlation between the results of this and other studies, as a result of both routine and definitions. These were similar to the majority of the studies, but both the duration of hospital stay (7.4 ± 4.1 days) and ICU were similar to those of patients who underwent only coronary revascularization at ICCOP. Bockeria et al. [21] demonstrated a time of hospital stay of 21.4 ± 6.9 days, in a group of patients with similar functional class and ventricular function of LV (EF), respectively (3.6 ± 0.5 x 3.5 ± 0.3) and (32.3 ± 9.2 x 32.9 ± 5.4%). However, the use of ventricular assist device, intra-aortic balloon was very different (14.3 x 58%), which may explain the difference in immediate mortality, in adittion to the group of Bockeria et al. [21] represents only a subgroup of their experience (14/224), which was removed the initial experience. These data differ from those presented by Gomes et al. [22], in a group of 11 patients in a limited period in which there was no mortality or use of circulatory assistance.
The immediate mortality was actually a significant factor in relation to world literature, when compared with the EuroSCORE, with an increased relative risk (OR) of 0.75% and 6.1% absolute. When attempting to assess the reason for this discrepancy, it was not possible to reach a clinical conclusion, and for this we analyzed - through multiple linear regression - factors that could influence mortality. The variable highlighted was the ejection fraction less than 32.31% (P = 0.0284); when analyzing the the linear regression of three most significant variables, functional class, LV ejection fraction, and time of anoxic cardiac arrest, there was statistical significance of the last two, respectively with P equal to 0.0125 and 0.0713 (for times greater than 48.86 minutes). Adams et al. [23] demonstrated that, despite the EF s not a factor that counter-indicate this surgical technique, there were differences in its evolution, as well as the increased use of left ventricular assist. Athanasuleas et al. [16] in their study RESTORE also found EF less than 30% as one of the variables that influence the immediate mortality of these patients, together with the LVEDV, NYHA functional class and age. These authors showed, in relation to functional class, percentage from both pre- and postoperative similar to this study.
Despite the immediate mortality in this study exceeds the majority of the published studies, it is important to consider that this study included all patients, without exclude the mortality of the learning curve, and that the EuroSCORE in this group is greater than the studies with the same follow-up time and with similar EF [20]. Another factor that may have contributed to an immediate result with a high mortality is the lack of treatment of mitral valve dysfunction of patients in this group, recommended by some authors as being mandatory when performing this technique [24]. Suma et al. [25] presented immediate mortality in 54 patients, improvement in EF, LVESV and LVEDV and survival similar to this study group.
The concomitant coronary artery bypass procedure is a key factor for obtaining good results [19], especially when it is possible to graft the left anterior descending artery (LAD), not only for its relevance to the LV anterior wall, but mainly for the revascularization of septal branches. In this group, it was possible to bypass the LAD in 82.14% of the patients, being the LITA the graft of choice in 86.96% of them.
Survival at the end of 110 months of follow-up was of 54.7 ± 22.9% and is within the range of other groups, but the sample of patients at risk is small. When analyzing the survival after 5 years, 82.1 ± 7.2%, it is equal or greater than the majority of the studies [18,20,22,23], so we can affirm that patients who survived surgery presented a very good evolution.
There was a correlation between the improvement in echocardiographic values obtained within the last six months, and the quality of life obtained in the same period through the evaluation questionnaire. Despite improvement in echocardiographic parameters (40% in average), apparently, the improvement of the quality of life does not seem to be perceived both by the patient, referring to a general health condition. Only in the field of functional capacity, pain and limitation by emotional aspects presented significant improvement, but a persisting limitation by physical problems and vitality. In our country, one of the possibilities offered to explain this fact can be the irregular way that patients receive treatment and clinical follow-up without drug therapy optimization.
Study limitations
This retrospective study presents as the main limitation the total number of patients studied, and not performing, at the time, exams to mark the degree of heart failure, such as B-type natriuretic peptide (BNP), and myocardial necrosis, as troponin, which can damage the final analysis of risk factors for morbidity and mortality. Like other limiting factors, one should consider that only evaluation tests of the left ventricular parameters by echocardiography were performed, knowing that it would be ideal pre- and postoperative magnetic resonance imaging, for evaluation of volume, shape and ventricular function, as well as the sphericity index, and postoperative cineangiocoronariography for evaluation of coronary revascularization. Although we have performed an evaluation of quality of life for all survivors, in some cases (34.8%) information was obtained through contact with the assistant physician, which may not be optimal.
CONCLUSIONS
Reconstructive surgery of left ventricular geometry by endoventricular repair with septal exclusion, as surgical technique for remodeling treatment, after myocardial ischemia, presented high immediate mortality, dependent on the preoperative left ventricular ejection fraction, but with excellent survival at the end of 111 months of follow-up. Factors that contributed to an unfavorable immediate result were: 1) at short-term, the left ventricular ejection fraction less than 32.3%, 2) at long-term, females and the time of anoxic cardiac arrest over 48, 9 minutes. The relationship of improvement in echocardiographic postoperative findings was consistent with the improvement of quality of life of patients, although a smaller proportion than expected in some areas.
ACKNOWLEDGMENTS
To Full Professor João Carlos Leal, for his help in the formulation and discussion of statistics in this article.
2. Murali S. Long-term circulatory support - the left ventricular assist system for advanced heart failure. Business Briefing: US Cardiology;2004:1-4.
3. Shah PJ, Hare DL, Raman JS, Gordon I, Chan RK, Horowitz JD, et al. Survival after myocardial revascularization for ischemic cardiomyopathy: a prospective ten-year follow-up study. J Thorac Cardiovasc Surg. 2003;126(5):1320-7. [MedLine]
4. Cooley DA, Collins HA, Morris GC Jr, Chapman DW. Ventricular aneurysm after myocardial infarction; surgical excision with use of temporary cardiopulmonary bypass. J Am Med Assoc. 1958;167(5):557-60. [MedLine]
5. Parolari A, Naliato M, Loardi C, Denti P, Trezzi M, Zanobini M, et al. Surgery of left ventricular aneurysm: a meta-analysis of early outcomes following different reconstruction techniques. Ann Thorac Surg. 2007;83(6):2009-16. [MedLine]
6. Jatene AD. Left ventricular aneurysmectomy. Resection or reconstruction. J Thorac Cardiovasc Surg. 1985;89(3):321-31. [MedLine]
7. Dor V, Saab M, Coste P, Kornaszewska M, Montiglio F. Left ventricular aneurysm: a new surgical approach. Thorac Cardiovasc Surg. 1989;37(1):11-9. [MedLine]
8. Cooley DA. Ventricular endoaneurysmorrhaphy: a simplified repair for extensive postinfarction aneurysm. J Cardiac Surg. 1989;4(3):200-5.
9. Mickleborough LL, Maruyama H, Liu P, Mohamed S. Results of left ventricular aneurysmectomy with a tailored scar excision and primary closure technique. J Thorac Cardiovasc Surg. 1994;107(3):690-8. [MedLine]
10. Almeida RMS, Lima Jr JD, Bastos LC, Carvalho CT, Loures DR. Remodelamento do ventrículo esquerdo pela técnica da endoventriculoplastia com exclusão septal: experiência inicial. Rev Bras Cir Cardiovasc. 2000;15(4):302-7. View article
12. Prates PR, Homsi Neto A, Lovato LM, Teiseira GF, Sant'Anna JR, Yordi LM, et al. Late results of endoventricular patch plasty repair in akinetic and dyskinetic areas after acute myocardial infarction. Arq Bras Cardiol. 2002;79(2):107-16. [MedLine]
13. Ciconelli RM, Ferraz MB, Santos W, Meinão I, Quaresma MR. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Rev Bras Reumatol. 1999;39(3):143-50.
14. Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, et al. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006;113(11):1424-33. [MedLine]
15. Tulner SA, Bax JJ, Bleeker GB, Steendijk P, Klautz RJ, Holman ER, et al. Beneficial hemodynamic and clinical effects of surgical ventricular restoration in patients with ischemic dilated cardiomyopathy. Ann Thorac Surg. 2006;82(5):1721-7. [MedLine]
16. Athanasuleas CL, Buckberg GD, Stanley AW, Siler W, Dor V, Di Donato M, et al. Surgical ventricular restoration in the treatment of congestive heart failure due to post-infarction ventricular dilation. J Am Coll Cardiol. 2004;44(7):1439-45. [MedLine]
17. Menicanti L, Di Donato M. The Dor procedure: what has changed after fifteen years of clinical practice? J Thorac Cardiovasc Surg. 2002;124(5):886-90. [MedLine]
18. Dor V, Di Donato M, Sabatier M, Montiglio F, Civaia F. Left ventricular reconstruction by endoventricular circular patch plasty repair: a 17-year experience. Semin Thorac Cardiovasc Surg. 2001;13(4):435-47. [MedLine]
19. Schinkel AF, Poldermans D, Rizzello V, Vanoverschelde JL, Elhendy A, Boersma E, et al. Why do patients with ischemic cardiomyopathy and a substantial amount of viable myocardium not always recover in function after revascularization? J Thorac Cardiovasc Surg. 2004;127(2):385-90. [MedLine]
20. Sartipy U, Albage A, Lindblom D. The Dor procedure for left ventricular reconstruction. Ten-year clinical experience. Eur J Cardiothorac Surg. 2005;27(6):1005-10. [MedLine]
21. Bockeria LA, Gorodkov AJ, Dorofeev AV, Alshibaya MD; RESTORE Group. Left ventricular geometry reconstruction in ischemic cardiomyopathy patients with predominantly hypokinetic left ventricle. Eur J Cardiothorac Surg. 2006;29(Suppl 1):S251-8. [MedLine]
22. Gomes WJ, Jaramillo JI, Asanuma F, Alves FA. Reconstrução fisiológica do ventrículo esquerdo: o conceito de máxima redução ventricular e mínima resposta inflamatória. Rev Bras Cir Cardiovasc. 2004;19(4):353-7. View article
23. Adams JD, Fedoruk LM, Tache-Leon CA, Peeler BB, Kern JA, Tribble CG, et al. Does preoperative ejection fraction predict operative mortality with left ventricular restoration? Ann Thorac Surg. 2006;82(5):1715-9.
24. Barletta G, Toso A, Del Bene R, Di Donato M, Sabatier M, Dor V. Preoperative and late postoperative mitral regurgitation in ventricular reconstruction: role of local left ventricular deformation. Ann Thorac Surg. 2006;82(6):2102-9. [MedLine]
25. Suma H, Isomura T, Horii T, Hisatomi K. Left ventriculoplasty for ischemic cardiomyopathy. Eur J Cardiothorac Surg. 2001;20(2):319-23. [MedLine]
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license