Lino Sergio Rocha ConceiçãoI,II,III; Caroline Oliveira GoisI,II,III; Raiane Eunice Santos FernandesI,II,III; Paulo Ricardo Saquete Martins-FilhoIV; Mansueto GomesV; Victor Ribeiro NevesVI; Vitor Oliveira CarvalhoI,II,III
DOI: 10.21470/1678-9741-2019-0420
ABSTRACT
Introduction: Heart transplantation (HTx) is the gold standard procedure for selected individuals with refractory heart failure. High-intensity interval training (HIIT) is safe and allows patients to exercise in high intensity for longer time when compared to moderate-intensity continuous training (MICT). The primary aim of this study was to perform a systematic review and meta-analysis about the effect of HIIT compared to MICT on exercise capacity, peak heart rate, and heart rate reserve in HTx recipients. Secondarily, we pooled data comparing MICT and no exercise training in these patients.ACT = Active recovery
AIT = Aerobic interval training
CI = Confidence interval
F = Female
HIIT = High-intensity interval training
HR = Hear rate
HRQoL = Health-related quality of life
HTx = Heart transplantation
M = Male
MD = Mean difference
MICT = Moderate-intensity continuous training
NR = Not reported
PeakVO2 = Peak oxygen consumption
RCTs = Randomized controlled trials
SD = Standard deviation
SDc = Standard deviation of change
SE = Standard error
INTRODUCTION
Heart transplantation (HTx) is the gold standard procedure for selected individuals with end-stage heart failure[1]. Even knowing that HTx improves patients’ exercise tolerance, it is not restored to normal values[2]. The concern about exercise tolerance in HTx recipients is based on the association between peak oxygen consumption (peakVO2), the gold standard method to assess cardiorespiratory fitness, and survival[3,4].
Several studies have demonstrated the positive effects of aerobic exercise training on peakVO2 in HTx recipients[5-7]. However, there is no consensus on how, when, or at what intensity exercise should be performed by HTx patients[8]. High-intensity interval training (HIIT) allows patients to exercise in higher intensity when compared to standard continuous training. A previous well performed meta-analysis[9] showed that HIIT was safe and effective in improving peakVO2 in HTx recipients when compared to no training. However, the lack of studies that compared HIIT with moderate-intensity continuous training (MICT) limited the previous meta-analysis. Moreover, conflicting results about HIIT superiority are still under discussion in cardiovascular rehabilitation[10,11].
Since the previous meta-analysis was published[9], new randomized controlled trials (RCTs) comparing HIIT with MICT were published[12,13]. Due to the new available data, the primary aim of the present study was to perform a systematic review and meta-analysis to synthesize evidence about the effect of HIIT compared to MICT on exercise capacity, peak heart rate, and heart rate reserve in HTx recipients. Secondarily, we pool data from trials comparing HIIT and no exercise training in these patients.
METHODS
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement[14] and supplemented by guidance from the Cochrane Collaboration Handbook for Systematic Reviews of Interventions[15]. A flow diagram showing the reference screening and study selection is presented on Figure 1.
Eligibility Criteria
To establish the eligibility criteria we used the following PICOT elements (standing for Participants, Intervention, Comparison, Outcomes, and Study type): Population, HTx recipients; Intervention, HIIT; Comparison, MICT or no exercise training; Primary outcome, peakVO2 (ml/kg/min); Secondary outcomes, peak heart rate and heart rate reserve (bpm); Study type, RCTs.
Search Strategy
We searched for references in PubMed, Scopus, and Cochrane Central Register of Controlled Trials up to February 2019. A gray literature search included Google Scholar and OpenThesis. The first 100 results of the Google Scholar search were analyzed. The search was limited to studies published in full-text versions, without language restriction. Search strategy is provided in the online supplement. The reference lists of all eligible studies and reviews were also scanned to identify additional studies for inclusion. The authors were contact by e-mail for confirmation of any data or additional information if needed.
Quality of the Studies
Risk of bias was assessed according to the Cochrane guidelines for RCTs. Seven domains were assessed for evaluation: sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other potential sources of bias (Figure 2). Risk of bias was rated as low, unclear, or high according to established criteria (Figure 3)[16].
Data Collection and Analysis
Two independent reviewers (COG and RESF) searched for relevant studies according to title and abstract. If at least one of the reviewers considered one reference eligible, the full text was obtained for a complete assessment. Then, the two reviewers assessed the full text according to the eligibility criteria. Thereafter, the following information from the studies were extracted: demographic characteristics of study participants, exercise protocols, adverse events, and outcome data. Values (mean difference [MD] and standard deviation [SD]) for peakVO2, peak heart rate, and heart rate reserve were extracted before and after intervention.
The meta-analysis was performed using the change between pre- and post-intervention means for each intervention group and the change SD calculated. If the SD of change [SDc]) for a given outcome was not reported, the formula:
was applied. SDpre, SDpost, and corrpre,post represent the SD of the pre-intervention value, the SD of the post-intervention value, and the correlation coefficient between pre- and post-intervention values, respectively. The corrpre,post was conservatively set at 0.5. Mean changes were pooled using the random-effects, generic inverse variance method. A forest plot was used to graphically present the effect sizes and the 95% confidence intervals (CIs). A two-tailed P-value of <0.05 was used to determine significance. Statistical heterogeneity was assessed by using the Cochran Q test[17] and quantified by the I2 index[18]. We conducted all analyses using Review Manager 5.3 (Cochrane IMS, Copenhagen, Denmark).
RESULTS
Studies Characteristics
Five RCTs[5,12,13] (total of 212 HTx recipients with mean age of 57 years) were included in this systematic review. Exercise protocols were well reported (Tables 1 and 2). Follow-up periods were also well reported among studies: eight weeks[17,18], 12 weeks[19,20], and one year[8]. No serious adverse events were reported by the studies. In general, the studies presented a low/uncertain risk of bias. Figure 3 presents results of individual assessment by Cochrane risk of bias.
| Study | Disease | Sample size (including dropouts) | Gender | Age (years) | Time after transplantation | Outcomes | Key findings | Dropouts (%) | Dropouts before and after intervention |
|---|---|---|---|---|---|---|---|---|---|
| Nytrøen et al.[8], 2019 | HTx | 81 | M (66)/F (15) | 50 | 3 months | PeakVO2, HRQoL, left ventricular function, endothelial function, and biomarkers | HIIT group demonstrated greater improvements than those observed in the MICT group (mean difference: 1.8 ml/kg/min) | 3.8% | 3.8% |
| Dall et al.[13], 2014 | HTx (normal chronotropic response and chronotropic impairment) | 20 (16) | M (12)/F (4) | 51.9 | 6.4 years | PeakVO2, blood pressure, HRpeak, HRrest, HRreserve, HRrecovery, workload | There was an improve in peakVO2 (0,001), HRpeak (0,014), and HRreserve (0,012) | All - 3 (20%) | It was a crossover study. NR |
| Nytrøen et al.[18], 2012 | HTx | 57 (52) | M (33)/F (15) | 51 | 4.1 years | Exercise capacity (peakVO2 and peakVO2 predicted), body composition, biochemistry, and HRQoL | HIIT improved peakVO2 (0.001), HRreserve (0,002), HRpeak (0.035) | All - 9 (15%) | HIIt - 2 (8%), control group - 2 (8%) |
| Hermann et al.[19], 2011 | HTx | 30 (27) | M (22)/F (5) | 50 | 6,9 years | PeakVO2, endothelial function, blood pressure, markers of inflammation | PeakVO2 was higher in the HIIT group (0,001), flow-mediated vasodilation (0,048), reduced blood systolic pressure (0,03), reduced plasma levels (0,02) | All - 3 (10%) | HIIT - 2 (6,7%), control group - 1 (3,3%) |
| Study | Type of exercise | VO2measurement | Intensity | Trained intensity | Volume | Frequency (´ per week) | Length (weeks) | Supervision |
|---|---|---|---|---|---|---|---|---|
| Nytrøen et al.[8], 2019 | HIIT (AIT) | Cardiopulmonary test | 81-93% peak effort | 10 min warm-up4 bouts (4 min of HIIT) and 3 bouts (3 min of MICT)5 min cooldown | 3 | 02/mar | 39 | Nytrøen et al., 2019 |
| MICT (ACT) | Cardiopulmonary test | 60-80% peak effort | 10 min warm-up | 3 | 02/mar | 39 | ||
| 25 min exercise | ||||||||
| 5 min cooldown | ||||||||
| Dall et al.[13], 2014 | HIIT (AIT) | Cardiopulmonary test | > 80%peakVO2 | 10 min warm-up | 3 | 3 | 12 | Dall et al., 2014 |
| 16 min exercise | ||||||||
| 10 min cooldown | ||||||||
| MICT (ACT) | Cardiopulmonary test | 60-70% peakVO2 | 10 min warm-up | 3 | 3 | 12 | ||
| 45 min exercise | ||||||||
| 10 min cooldown | ||||||||
| Hermann et al.[19], 2011 | HIITa | Cardiopulmonary test | 80%, 85%, and 90% of peakVO2 | 10 min warm-up | 3 | 3 | 8 | Hermann et al., 2011 |
| 42 min exercise | ||||||||
| 10 min cooldown | ||||||||
| Control group (sedentary?) Only education | Cardiopulmonary test | NR | NR | NR | NR | NR | ||
| Nytrøen et al.[18], 2012 | HIIT | Cardiopulmonary test | 85-95% HRmax | 10 min warm-up | 3 | 3 | 8 | Nytrøen et al., 2012 |
| 16 min exercise | ||||||||
| NR cooldown | ||||||||
| Control group (no intervention) | Cardiopulmonary test | NR | NR | NR | NR | NR | ||
| Haykowsky et al.[5], 2009 | HIIT | Cardiopulmonary test | 60-80% peakVO2 | 10 min warm-up | 3 | 5´/week (12 weeks) | 12 | Nytrøen et al., 2013 |
| 16 min exercise | ||||||||
| NR cooldown | ||||||||
| Control group (no intervention) | Cardiopulmonary test | NR | NR | NR | NR | NR |
Overall Analysis
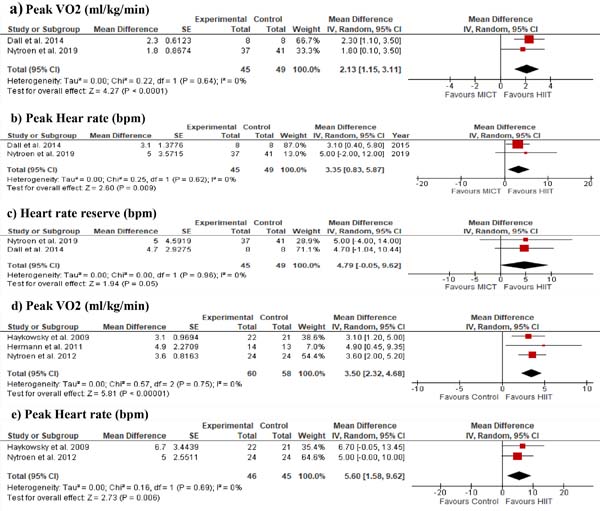
HIIT improved peakVO2 (MD = 2.1; 95% CI 1.1, 3.1; P<0.0001) (Figure 4A), peak heart rate (MD = 3.4; 95% CI 0.8, 5.9; P=0.009) (Figure 4B), and heart rate reserve (MD = 4.8; 95% CI -0.05, 9.6; P=0.05) (Figure 4C) compared to MICT. Improvements on peakVO2 (MD = 3.5; 95% CI 2.3, 4.7; P<0.00001) (Figure 4D) and peak heart rate (MD = 5.6; 95% CI 1.6, 9.6; P=0.006) (Figure 4E) were also found comparing HIIT and no exercise training. No data was available to compare heart rate reserve between HIIT and control without exercise. No between-study heterogeneity (I2 = 0%) was found in the meta-analyses.
DISCUSSION
Our systematic review found that HIIT was superior than MICT on peakVO2, peak heart rate, and heart rate reserve in HTx recipients. In recent years, a growing number of studies have suggested that HIIT is similar or even superior to MICT in peakVO2, heart rate response, and quality of life improvements[8,13,21].
A previous meta-analysis reported the efficiency of HIIT on peakVO2 gains in HTx when compared to no exercise training[9]. However, our meta-analysis contributes to a better understanding of the effect size of HIIT when compared with the standard exercise intensity prescription (MICT). Additionally, some issues regarding the effects of exercise protocols must be addressed in relation to the apparent superiority of HIIT over MICT. In a recent review, Dun et al.[22] argued that the exercise duration and ratio of high and low-intensity bouts are key factors that differentiate HIIT from MICT and may contribute to the patient's response. In general there are three main protocols of HIIT: long, medium, and short. The long-duration HIIT protocol (four minutes at high intensity - 85-95% peakVO2 - and three minutes at moderate intensity - 60-70% of peakVO2) is the most widely used in patients with cardiovascular diseases. Another meta-analysis demonstrated that the long-duration HIIT protocols were associated with larger improvements in peakVO2 in healthy individuals[23]. In our meta-analysis, the studies comparing HIIT to MICT used long-duration HIIT protocol. This may be one of the main factors behind the superiority of HIIT over MICT[22].
The concept of isocaloric protocol must also be considered when HIIT and MICT are compared. The superiority of HIIT over MICT disappeared when studies that used isocaloric protocols were analyzed in previous meta-analyses involving patients with coronary artery disease[11] and heart failure[10]. In our analysis, only one study[23] reported isocaloric protocol, which limits any pragmatic conclusion about HIIT superiority.
Additionally, our secondary analysis demonstrated that HIIT had superior effects to MICT in peak heart rate and heart rate reserve. In four of the five included studies, the mean time after transplantation was between four and six years[13,16-18]. Initially, we supposed that this superiority would be associated with cardiac reinnervation. Long-term HTx recipients are expected to show some degree of cardiac reinnervation, which nearly normalizes heart rate control. In contrast, newly HTx recipients display a denervated status and the heart rate response is markedly reduced compared to health individuals. On the other hand, in one study, HTx recipients were followed 8-12 weeks after HTx[12]. The apparent superiority of HIIT may be associated with the volume of training[23]. Additionally, the small number of studies and of isocaloric protocols does not allow us to fully support the superiority of HIIT over MICT in cardiac dynamics.
Limitation
Caution is warranted in interpreting the results of this study. One important limitation is the low number of studies comparing HIIT to MICT and the lack of isocaloric protocols. Another important limitation is that in just one study[13] the patients were followed by a physical therapist in a 1:1 setting. This type of setting may guarantee that the patients reach the proper intensity prescribed. On the other hand, this type of setting may not be suitable in most cardiac rehabilitation centers around the world, especially in middle- and lower-income countries.
CONCLUSION
In conclusion, current available evidence suggests that HIIT is superior to MICT on peakVO2, peak heart rate, and heart rate reserve improvements in HTx recipients. However, new RCTs are necessary to analyze the influence of isocaloric protocols and different duration protocols on peakVO2 in HTx recipients.
REFERENCES
1. Harris C, Cao C, Croce B, Munkholm-Larsen S. Heart transplantation. Ann Cardiothorac Surg. 2018;7(1):172. doi:10.21037/acs.2018.01.11.
2. Lavie CJ, Arena R, Earnest CP. High-intensity interval training in patients with cardiovascular diseases and heart transplantation. J Heart Lung Transplant. 2013;32(11):1056-8. doi:10.1016/j.healun.2013.08.001.
3. Yardley M, Havik OE, Grov I, Relbo A, Gullestad L, Nytrøen K. Peak oxygen uptake and self-reported physical health are strong predictors of long-term survival after heart transplantation. Clin Transplant. 2016;30(2):161-9. doi:10.1111/ctr.12672.
4. Anderson L, Nguyen TT, Dall CH, Burgess L, Bridges C, Taylor RS. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4(4):CD012264. doi:10.1002/14651858.CD012264.pub2.
5. Haykowsky M, Taylor D, Kim D, Tymchak W. Exercise training improves aerobic capacity and skeletal muscle function in heart transplant recipients. Am J Transplant. 2009;9(4):734-9. doi:10.1111/j.1600-6143.2008.02531.x.
6. Tomczak CR, Tymchak WJ, Haykowsky MJ. Effect of exercise training on pulmonary oxygen uptake kinetics in heart transplant recipients. Am J Cardiol. 2013;112(9):1489-92. doi:10.1016/j.amjcard.2013.06.037.
7. Kobashigawa JA, Leaf DA, Lee N, Gleeson MP, Liu H, Hamilton MA, et al. A controlled trial of exercise rehabilitation after heart transplantation. N Engl J Med. 1999;340(4):272-7. Erratum in: N Engl J Med 1999;340(12):976. doi:10.1056/NEJM199901283400404.
8. Nytrøen K, Rolid K, Andreassen AK, Yardley M, Gude E, Dahle DO, et al. Effect of high-intensity interval training in De Novo heart transplant recipients in Scandinavia. Circulation. 2019;139(19):2198-211. Erratum in: Circulation. 2019;140(17):e737. doi:10.1161/CIRCULATIONAHA.118.036747. [MedLine]
9. Perrier-Melo RJ, Figueira FAMDS, Guimarães GV, Costa MDC. High-intensity interval training in heart transplant recipients: a systematic review with meta-analysis. Arq Bras Cardiol. 2018;110(2):188-94. doi:10.5935/abc.20180017. [MedLine]
10. Gomes Neto M, Durães AR, Conceição LSR, Saquetto MB, Ellingsen Ø, Carvalho VO. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis. Int J Cardiol. 2018;261:134-41. doi:10.1016/j.ijcard.2018.02.076. [MedLine]
11. Gomes-Neto M, Durães AR, Reis HFCD, Neves VR, Martinez BP, Carvalho VO. High-intensity interval training versus moderate-intensity continuous training on exercise capacity and quality of life in patients with coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24(16):1696-707. doi:10.1177/2047487317728370. [MedLine]
12. Dall CH, Snoer M, Christensen S, Monk-Hansen T, Frederiksen M, Gustafsson F, et al. Effect of high-intensity training versus moderate training on peak oxygen uptake and chronotropic response in heart transplant recipients: a randomized crossover trial. Am J Transplant. 2014;14(10):2391-9. doi:10.1111/ajt.12873.
13. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-9, W64. doi:10.7326/0003-4819-151-4-200908180-00135.
14. Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions . Version 4.2.6. Chichester (UK): John Wiley & Sons, Ltd.; 2006 . 257 p. Available from:
15. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi:10.1136/bmj.d5928.
16. Cochran WG. The Combination of Estimates from Different Experiments. Biometrics. 1954;10(1):101-29. doi:10.2307/3001666.
17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-60. doi:10.1136/bmj.327.7414.557.
18. Nytrøen K, Rustad LA, Aukrust P, Ueland T, Hallén J, Holm I, et al. High-intensity interval training improves peak oxygen uptake and muscular exercise capacity in heart transplant recipients. Am J Transplant. 2012;12(11):3134-42. doi:10.1111/j.1600-6143.2012.04221.x.
19. Hermann TS, Dall CH, Christensen SB, Goetze JP, Prescott E, Gustafsson F. Effect of high intensity exercise on peak oxygen uptake and endothelial function in long-term heart transplant recipients. Am J Transplant. 2011;11(3):536-41. doi:10.1111/j.1600-6143.2010.03403.x.
20. Yardley M, Gullestad L, Bendz B, Bjørkelund E, Rolid K, Arora S, et al. Long-term effects of high-intensity interval training in heart transplant recipients: a 5-year follow-up study of a randomized controlled trial. Clin Transplant. 2017;31(1). doi:10.1111/ctr.12868.
21. Dun Y, Smith JR, Liu S, Olson TP. High-intensity interval training in cardiac rehabilitation. Clin Geriatr Med. 2019;35(4):469-87. doi:10.1016/j.cger.2019.07.011. [MedLine]
22. Bacon AP, Carter RE, Ogle EA, Joyner MJ. VO2max trainability and high intensity interval training in humans: a meta-analysis. PLoS One. 2013;8(9):e73182. doi:10.1371/journal.pone.0073182. [MedLine]
No financial support.
No conflict of interest.
Authors' roles & responsibilities
LSRC Drafting the work; final approval of the version to be published; leading author
COG Substantial contributions to the acquisition of data for the work; final approval of the version to be published
RESF Substantial contributions to the acquisition of data for the work; final approval of the version to be published
PRSMF Statistical analysis and Substantial contributions to the conception or design of the work.
MGN Substantial contributions to the analysis of data for the work; revising the work; final approval of the version to be published
VRN Drafting the work and revising it; final approval of the version to be published
VOC Substantial contributions to the acquisition of data for the work; drafting the work; final approval of the version to be published
Article receive on Thursday, May 23, 2019
Article accepted on Friday, April 17, 2020
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license