Gabriela Bertolini MatheusI; Desanka DragosavacII; Patrícia TrevisanIII; Cledycion Eloy da CostaIV; Maurício Marson LopesV; Gustavo Calado de Aguiar RibeiroVI
DOI: 10.5935/1678-9741.20120063
CG: control group
SG: study group
MIP: Maximal Inspiratory Pressure
MEP: Maximal Expiratory pressure
TV: tidal volume
VC: vital capacity, peak flow, peak expiratory flow
PO3: 3rd postoperative day
CPB: cardiopulmonary bypass
IMT: inspiratory muscle training
IMT: Inspiratory Muscle Trainer
PO1: 1st postoperative day
Preop.: preoperative
ANOVA: Analysis of variance
INTRODUCTION
Heart surgery can cause a number of complications, such as the postoperative pulmonary complications, with significant impact on morbidity and postoperative mortality and hospital spending.
The etiology is complex and multifactorial, involving physiological changes related to cardiopulmonary bypass (CPB), sternotomy mechanical changes, surgical manipulation, effects of anesthesia and mammary artery use, among other pre-, intra- and postoperative variables [1,2 ].
The patients who had undergone median sternotomy with mammary artery dissection and also presenting pleurotomy reduction in ventilatory variables, in addition, factors such as immobility in bed, pain and temporary dysfunction of the diaphragm contribute to the hypoxemia, and pulmonary dysfunction in the postoperative period [3,4].
It is common to observe changes in lung mechanics, restrictive breathing pattern and shallow breathing postoperatively. The atelectasis is common and is associated with reduced lung capacity and respiratory muscle strength. Also pneumonias can occur with an incidence reported in the literature between 3% and 16% [5].
Given the presentation of pulmonary dysfunction associated with cardiac surgery and its possible repercussions, it is crucial more research about the resources available today to reverse this situation [6].
Respiratory therapy is an integral part in managing the care of cardiac patients, both in pre- and postoperatively, it contributes significantly to better prognosis, acting preoperatively (Pre-op) with techniques aimed at the preventing pulmonary complications, and postoperatively, with hygiene and pulmonary expansion maneuvers [7].
In view of the described above, this study aimed to assess the ventilatory capacity in postoperative patients undergoing CABG and compare the values of the performance measures of respiratory muscles through the maximal inspiratory pressure (MIP), maximal expiratory pressure (MEP), tidal volume (TV), vital capacity (VC) and peak expiratory flow between a group undergoing conventional physiotherapy, and another group undergoing respiratory muscle training with threshold® Inspiratory Muscle Trainer (IMT).
METHODS
From November 2007 to October 2008, 199 heart surgeries were performed at Hospital e Maternidade Celso Pierro, and 122 patients underwent CABG. Of these, were excluded during preoperative those presenting arrhythmias, chronic obstructive pulmonary disease, identified by prior spirometry or under use of bronchodilators, patients using tridil, and those presenting anginal chest pain and patients with a body mass index greater than 30 kg/m2. We also excluded patients who had complications in the postoperative period, of whom did not allow the measurement of weights on first postoperative (PO1) day under use of intra-aortic balloon, emergency surgery, reoperations and patients undergoing procedures associated with revascularization.
The study was approved by the Research Ethics Committee of the State Campinas and Pontifical Catholic University of Campinas, under registration number 294/2005 and 857/07, according to the Declaration of Helsinki. All patients signed a written informed consent form. The research was recorded in CONEP under number 163.623.
They were randomized into two groups randomly 47 patients: 23 patients in the study group (SG) and 24 patients in the control group (CG), diagnosed with chronic coronary failure and undergoing elective CABG with cardiopulmonary bypass via median sternotomy.
The surgical risk stratification was performed using the EuroSCORE, SG 0.71 ± 0.0018 and CG 0.76 ± 0.0029 [8].
The anesthetic protocol and surgical technique, including the protocol for conduct of CPB were the same. All patients underwent median sternotomy using internal mammary artery graft, complemented with saphenous vein grafts, as inclusion criteria, and had a drain on subxiphoid position and another inserted in the sixth intercostal space to drain the left pleura. Analgesia in the postoperative period was optimized and followed the standard protocol used at the hospital. The CG underwent physiotherapy protocol service, which consists of assessment and guidance in preoperative, pulmonary reexpansion with fractionated patterns, incentive spirometry, orthostatic and postoperative ambulation, twice a day. The experimental group underwent the same protocol and also the inspiratory muscle training (IMT) using threshold® IMT twice a day with three sets of 10 repetitions with 40% of MIP measured on fist postoperative day.
IMT Respironics® Threshold® is a device having a valve closed by positive pressure with a spring that produces linear load independent stream, and was used for the IMT. The IMT was performed daily during the first three postoperative days, with three sets of ten repetitions, twice a day. The load used was 40% of the MIP measured in PO1 and rhythm and pauses were determined for each patient.
We assessed MIP, MEP, TV, VC and peak expiratory flow (peak flow), in three stages, Preoperative, PO1 and 3rd postoperative day (PO3), after performing the last training.
All measures were explained and experienced by patients before the trial and considered the best of three attempts. The MIP was performed using manovacuometer from functional residual capacity and MEP from total lung capacity, with values close to each other, without perioral leak, and the highest value obtained was considered [9]. The TV was measured using spirometer through the minute volume and divides by respiratory rate measured within one minute, the VC was measured using spirometer, from total lung capacity, with a slow and prolonged expiration.
The airway permeability was assessed by measuring the peak flow achieved with maximum and fast expiratory effort maneuver, starting from a maximal inspiration. The recordings were made through the Peak Flow Meter (ASSESS ®) device, which provided the peak expiratory flow in liters per minute.
Statistical Analysis
To compare proportions, we used the chi-square test or Fisher exact test. In the comparison of continuous or sortable variables in a single time between two groups we used the Mann-Whitney test. To study the effect of time and groups in the assessed parameters analysis of variance (ANOVA) was used for repeated measures and contrast profile for evolution of time. Results were considered statistically significant when P <0.05.
RESULTS
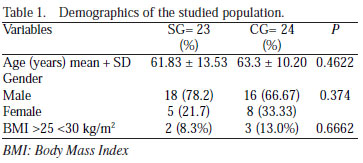
The groups were similar with respect to demographics and comorbidities (Tables 1 and 2).

There was no statistically significant difference between groups with respect to time of surgery [CG 4.76 ± 0.73 hours and SG 4.36 ± 0.80 hours (P = 0.119)] CPB [CG 72.42 ± 17, 77 minutes and SG 75.78 ± 23.08 minutes (P = 0.658)], and time on which patients remained on mechanical ventilation [CG 2.43 ± 2.51 hours and SG 1.75 ± 2.80 hours (P = 0.256)] after admission to the coronary care unit (Table 3).

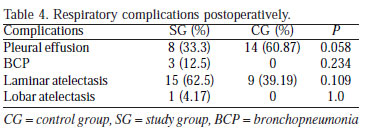
We considered the respiratory complications regardless of the degree and intensity of involvement. For the diagnosis the radiological report of the first three postoperative days was considered. In this study, there was no statistically significant difference between the groups when the presence of respiratory complications. Regarding the presence of pleural effusion, 14 (60.87%) patients in the SG and eight (33.3%) in the CG showed that complication, found in chest radiography with opacification of the costophrenic angle, between PO1 and PO3. Laminar atelectasis was detected in nine (39.13%) of the patients in SG and 15 (62.5%) of CG. Lobar atelectasis was not observed in any patient of SG, and was observed in one (4.17%) of CG, and pneumonia in any patient of SG, and three (12.5%) of CG (Table 4).
The group undergoing respiratory training showed a significant difference in length of stay in the coronary care unit, but with no difference between groups in length of hospital stay (Table 5).

Maximal Respiratory Pressures
When comparing the MIP in the 1st PO with Preoperative, a decrease in both groups was found, CG [-60.21 ± 24.65 cmH2O vs. -85.71 ± 28.46 cmH2O] and SG [-47.57 ± 18.54 cmH2O vs. -81.91 ± 24.81 cmH2O (P< 0.0001)]. In PO3 was observed significant recovery of MIP measures, but no return to preoperative values [GC -75.75 ± 25.00 cmH2O and GE -66.43 ± 21.79 cmH2O (P<0.0001)]. There was no significant difference between CG and SG (P = 0.1680). The evolution of the MIP values can be seen in Figure 1.

Comparing the MEP values in PO1 and Preoperative, there was significant reduction in both groups [CG 58.25 ± 27.96 cmH2O vs. 84.96 ± 31.51 cmH2O] and SG [61.04 ± 29.21 cmH2O vs. 94.70 ± 26.86 cmH2O (P< 0.0001)]. In PO3, there was an increase of measures [CG 70.04 ± 29.25 cmH2O and SG 78.39 ± 36.22 cmH2O (P<0.0001)], however, with no statistical difference between groups (P = 0.168 ). There was no return to preoperative values. The trend in the MEP values in the patients studied is shown in Figure 2.

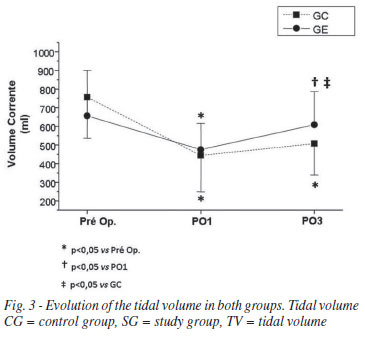
Tidal Volume Measures (TV)
Comparing the value of TV between PO1 and Preoperative, a decrease in both groups [CG 443.79 ± 195.10 vs. 756.38 ± 220.05 ml (P<0.0001)] and SG [475.17 ± 140.67 vs. 655.96 ± 244.42 ml (P=0.0004)]. In PO3, we observed a significant increase in the amount of TV in SG [608.09 ± 178.24 ml (P=0.0015)]. There were significant differences between CG and SG on the 3rd postoperative day (P=0.0490). The TV values in the studied patients are shown in Figure 3.
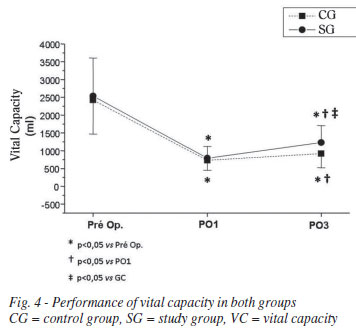
Vital Capacity (VC)
Comparing the VC value between PO1 and Preoperative, there was a decrease in both groups, CG [731.25 ± 279.68 ml vs. 2425.0 ± 956.33 ml (P<0.0001)] and SG [790.00 ± 330.45 ml vs. 2537.0 ± 1067.9 ml (P<0.0001)]. In PO3, we observed recovery of measures in both groups, but more markedly in the group undergoing respiratory training [CG 919.17 ± 394.47 ml and SG 1230.4 ± 477.86 ml]. There were significant differences between CG and SG (P=0.0222) in PO3. The measures remained significant decreased with respect to preoperative value. The VC values of the studied patients are shown in Figure 4.
Peak Expiratory Flow
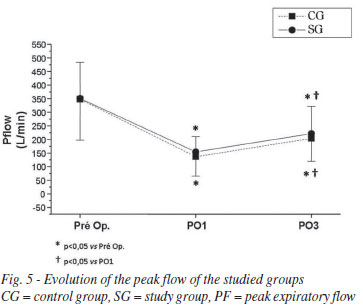
The peak flow value showed a significant reduction in PO1 when compared to preoperative [CG: 136.67 ± 71.18 L/m vs. 347.92 ± 150.51 L/m and SG: 154.13 ± 56.34 L/m vs. 350.65 ± 133.19 L/m (P<0.0001)], with no difference between groups (P=0.4750). In PO3, measures of CG 203.75 ± 83.55 L/m and SG 221.30 ± 100.87 L/m showed significant recovery, but did not return to the preoperative values. The development of measures of peak flow is shown in Figure 5.
DISCUSSION
Regarding the descriptive characteristics of the study population, the groups were similar in age, gender and weight. Several authors performed measurements of maximal respiratory pressures and the values published in the form of equations, used as reference for certain populations. Most of these authors relate the values of maximal respiratory pressures with age and gender [10].
In the present study, there was no significant difference between groups with respect to operative time, CPB and intubation. Surgery and anesthesia affect ventilatory function. Some authors observed an increase in lung density in areas dependent on both lungs after anesthesia, suggesting formation of areas of atelectasis [11]. According to Nardi et al. [12], CPB time greater than 60 minutes seems to have an inverse relationship with MIP values.
In this study there was no significant difference in relation to respiratory complications. Garcia & Costa [13] reported one or more types of pulmonary complications in the postoperative phase in 74% of patients, being 17% pleural effusion and 10% atelectasis.
Atelectasis is most frequently found in postoperative and radiological findings are key for the left lower lobe. Atelectasis is related to deterioration in gas exchange, decreased lung volumes and functional residual capacity and lung compliance. It becomes relevant when it is persistent, is associated with hypoxemia, increased breathing work and other signs of stress [14].
Landymore & Howell [15] reported that patients who received internal mammary artery as a graft and underwent chest drainage showed a higher incidence of pleural effusion, atelectasis in the left lower lobe and elevation of the left hemidiaphragm. Moreover, three months after surgery these patients maintained loss of lung volume, areas of atelectasis and pleural effusion. In this study, all patients received internal thoracic artery graft, being that fact uniformed.
In this study, all variables, MIP, MEP, peak expiratory flow, TV and VC, presented a significant reduction in PO1 compared to preoperative.
A significant reduction in postoperative respiratory muscle performance is expected, as shown by lower values of MIP and MEP in both groups. The effects of cardiac surgery on muscle function, pain and the presence of chest tubes probably contribute to these findings. In the postoperative period, there is a reduction in lung volumes and capacities, and impaired respiratory function [12].
The reduction in the amount of peak expiratory flow indicates interference in respiratory function, by decreasing muscle strength and range of motion, secondary to surgical trauma [13]. Similar results were reported by Johnson et al. [5] in patients during postoperative CABG.
Also Nardi et al. [12] reported a significant reduction of approximately 50% for all variables (VC, MIP, MEP and peak expiratory flow) in the PO1 of heart surgery when compared with the preoperative period.
In this study, there were significant increases in all measured variables until the PO3 in both groups.
Despite the increase, there was no recovery of measures to preoperative values, except for the TV value in the trained group. This finding is in agreement with data shown by Silva et al. [16] who assessed the behavior of MIP, MEP and spirometry in a group of patients undergoing cardiac surgery and found significant reductions in lung volumes and flows and in maximal respiratory pressures in PO1. There was a significant increase in respiratory muscle strength until hospital discharge, even without specific training, however, the measures remained below the values obtained in the preoperative [16].
In this study, although the inspiratory muscle training has not demonstrated effects on MIP and MEP until PO3, it was effective in increasing, significantly, ventilatory function, as demonstrated by the increase in the TV and VC values, the group who underwent training with.
Ferreira et al. [17] reported similar results after training with IMT® threshold in preoperative. The patients showed a significant increase in forced vital capacity and maximum voluntary ventilation, but no difference in MIP and MEP was observed in the postoperative period.
The more frequent result of the change in lung volume in patients with muscle weakness is the fall in vital capacity. Thus, it can be noted that the VC reflects the weakness of respiratory muscles and lungs static mechanical load. [18]
Changes in pulmonary function in patients undergoing cardiac surgery with CPB are largely responsible for the morbidity of these patients. The atelectasis are the most common complications, caused by decreased functional residual capacity, changes on chest wall mechanics and lung tissue, by increasing airway resistance and the postoperative pain, among other factors [19].
In this study, the control group received no specific training on respiratory muscles, but were also oriented in the preoperative and underwent respiratory therapy after surgery, and were encouraged to get out of bed and ambulate early.
It is possible that these measures and exercises, even without load, have contributed to improving the variables in the control group.
Barros et al. [20] trained a group of patients with 40% of MIP, from PO1 until discharge, which occurred on the 7th postoperative day. The behavior of MIP, MEP, TV and peak expiratory flow, as in the present study, significantly declined, but returned to the values obtained in the preoperative at the time of hospital discharge.
Other studies have shown that the respiratory muscle training during preoperative is effective to increase respiratory muscle strength in patients undergoing cardiac surgery [17,21,22].
Leguisamo et al. [23] reported that patients oriented in the Preoperative are better prepared to collaborate with the needs of postoperative treatment. Understanding the aim of pre- and postoperative physiotherapy, the limitations resulting from the surgical process and the proposed physiotherapy technique may help in the recovery and thereby reduce the length of stay in hospital.
Although the effects of respiratory muscle training are well defined with regard to the benefits to the patient, some methodological issues remain controversial in relation to the load to be applied, number of repetitions and training period.
In this study, the positive benefit of inspiratory muscle training can be observed through the significant increase in tidal volume, in PO3, with return to preoperative value. There was also a significant increase in TV in the control group, despite the variable remains below the value obtained in preoperative. This result reinforces the findings of other authors who applied muscle training for a longer period and obtained an increase in MIP and MEP.
It is possible that by applying muscle training for a few more days, such a result could have been obtained.
Measuring and monitoring the function of the respiratory muscles through the MIP and MEP measurements in patients undergoing cardiac surgery is a simple and important for planning interventions that can bring clinical benefits such as reduced postoperative pulmonary complications.
In this context, it is suggested that further studies be performed in order to investigate and better define the methodology for obtaining the positive benefits of respiratory muscle training described herein.
The limitations of this study are related to measures of MIP and MEP, TV, VC, and peak expiratory flow assessment. These tests depend on the understanding and cooperation of participating individuals. Therefore, the technique can have a determinative positive effect on the outcome.
CONCLUSION
Patients undergoing CABG presented a significant reduction of the performance measures of respiratory muscles in PO1 when compared to baseline Preoperative. The respiratory muscle training was effective in recovering the TV and VC in PO3 in the group undergoing training. There was no difference in the presence of pulmonary complications and length of hospital stay between groups.
REFERENCES
1. Weissman C. Pulmonary function after cardiac and thoracic surgery. Anesth Analg. 1999;88(6):1272-9. [MedLine]
2. Wynne R, Botti M. Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care. 2004;13(5):384-93. [MedLine]
3. Guizilini S, Gomes WJ, Faresin SM, Carvalho ACC, Jaramillo JI, Alves FA, et al. Efeitos do local de inserção do dreno pleural na função pulmonar no pós-operatório de cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2004;19(1):47-54. View article
4. Wimmer-Greinecker G, Yosseef-Hakimi M, Rinne T, Buhl R, Matheis G, Martens S, et al. Effect of internal thoracic artery preparation on blood loss, lung function, and pain. Ann Thorac Surg. 1999;67(4):1078-82. [MedLine]
5. Johnson D, Kelm C, To T, Hurst T, Naik C, Gulka I, et al. Postoperative physical therapy after coronary artery bypass surgery. Am J Respir Crit Care Med. 1995;152(3):953-8. [MedLine]
6. Westherdahl E, Lindmark B, Eriksson T, Friberg O, Hedenstierna G, Tenling A. Deep-breathing exercices reduce atelectasis and improve pulmonary function after coronary artery bypass surgery. Chest. 2005;128(5):3482-8. [MedLine]
7. Cavenaghi S, Ferreira LL, Marino LHC, Lamari NM. Fisioterapia respiratória no pré e pós-operatório de cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc 2011;26(3):455-61. [MedLine] View article
8. Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9-13. [MedLine]
9. Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999;32(6):719-27. [MedLine]
10. Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969;99(5):696-702. [MedLine]
11. Lindberg P, Gunnarsson L, Tokics L, Secher E, Lundquist H, Brismar B, et al. Atelectasis and lung function in the postoperative period. Acta Anaesthesiol Scand. 1992;36(6):546-53. [MedLine]
12. Nardi C, Otranto CPM, Piaia IM, Forti EMP, Fantini B. Avaliação da força muscular, capacidades pulmonares e função pulmonar respiratória de pacientes submetidos à cirurgia cardíaca. In: 4ª Mostra Acadêmica e Congresso de Pesquisa da UNIMEP [on line]: 2006. Out,24-26. Piracicaba. Anais eletrônicos. Disponível em URL: http//www.unimep.br/phpg/mostraacademica/anais/4mostra/pdfs/171pdf.
13. Garcia RCP, Costa D. Treinamento muscular respiratório em pós-operatório de cirurgia cardíaca eletiva. Rev Bras Fisioter. 2002;6(3):139-46.
14. Renault JA, Costa-Val R, Rossetti MB. Fisioterapia respiratória na disfunção pulmonar pós-cirurgia cardíaca. Rev Bras Cir Cardiovasc. 2008;23(4):562-9. [MedLine]
15. Landymore RW, Howell F. Pulmonary complications following myocardial revascularization with the internal mammary artery graft. Eur J Cardiothorac Surg. 1990;4(3):156-61.
16. Silva BA, Pires de Lorenzo VA, Oliveira CR, Luzzi S. Comportamento da função pulmonar e da força muscular respiratória em pacientes submetidos à revascularização do miocárdio e à intervenção fisioterapêutica. RBTI. 2004;16(3):155-9.
17. Ferreira PEG, Rodrigues AJ, Évora PRB. Efeitos de um programa de reabilitação da musculatura inspiratória no pós-operatório de cirurgia cardíaca. Arq Bras Cardiol. 2009;92(4):275-82. [MedLine]
18. Oliveira RARA, Soares SMTP, Kousour C. Bases do treinamento muscular respiratório. In: Sarmento GJV, ed. O ABC da fisioterapia respiratória. 1ª ed. São Paulo: Manole; 2009. p.213-28.
19. Barbosa RAG, Carmona MJC. Avaliação da função pulmonar em pacientes submetidos à cirurgia cardíaca com circulação extracorpórea. Rev Bras Anestesiol. 2002;52(6):689-99. [MedLine]
20. Barros GF, Santos CS, Granado FB, Costa PT, Límaco RP, Gardenghi G. Treinamento muscular respiratório na revascularização do miocárdio. Rev Bras Cir Cardiovasc. 2010;25(4):483-90. [MedLine] View article
21. Hulzebos EH, Helders PJ, Favié NJ, De Bie RA, Brutel de la Riviere A, Van Meeteren NL. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA. 2006;296(15):1851-7. [MedLine]
22. Elias DG, Costa D, Oishi J, Pires VA. Efeito do treinamento muscular respiratório no pré e pós-operatório de cirurgia cardíaca. Rev Bras Ter Intens. 2000;12(1):9-18.
23. Leguisamo CP, Kalil RAK, Furlani AP. A efetividade de uma proposta fisioterapêutica pré-operatória para cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc 2005;20(2):134-41. View article
Article receive on Tuesday, April 10, 2012
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license