Andres Di Leoni Ferrari; Carolina Pelzer Süssenbach; João Carlos Vieira da Costa Guaragna; Jacqueline da Costa Escobar Piccoli; Guilherme Ferreira Gazzoni; Débora Klein Ferreira; Luciano Cabral Albuquerque; Marco Antonio Goldani
DOI: 10.5935/1678-9741.20110010
ABSTRACT
INTRODUCTION: Disturbances of the cardiac conduction system are potential complications after cardiac valve surgery.RESUMO
INTRODUÇÃO: Distúrbios do sistema de condução cardíaco são complicações potenciais e conhecidas dos procedimentos de cirurgia cardíaca valvar.INTRODUCTION
Disorders of cardiac conduction system are known and potential complications of the procedures for heart valve surgery. The incidence of disorders of atrioventricular (AV) in the post-cardiac surgery (POCS) valve is located, according to the literature, 10 to 15% [1]. Most patients have disturbances of a temporary nature and will require temporary cardiac pacing (DPM), but 1% to 3% of patients, given the irreversibility of the framework, will be subject to a definitive pacemaker (DPM) during hospitalization [ 1-3]. In this study, we analyzed the experience of more than 1100 valve surgery procedures in order to verify the relationship between factors pre-, intra-and postoperative (perioperative) associated with atrioventricular block (AVB) and the need for TAC with later implant DPM on POCS.
METHODS
Population and sample
From January 1996 to December 2008, 1,102 cardiac surgeries were performed at the Hospital São Lucas, Pontifical Catholic University of Rio Grande do Sul (PUC-RS), 718 (65.2%) aortic valve surgery and 407 (36.9 %) mitral valve surgery. Of these, 190 (17.2%) valve surgery (aortic or mitral) were combined with bypass surgery (CABG) and 23 (2.1%) multiple exchange surgery (aortic + mitral), the latter accounted for both surgery group in the aortic and mitral valve surgery.
Study design
Historical cohort observational study. Data were collected prospectively and entered into the database unit postoperatively in cardiac surgery at the Hospital São Lucas da PUC-RS.
Inclusion criteria
Patients aged over 18 years taken to heart valve surgery (replacement or repair) alone or combined with myocardial revascularization surgery.
Exclusion criteria
Tricuspid and pulmonary valve surgeries were excluded from the analysis when isolated due to the small number of patients undergoing these procedures. Also excluded were cases with incomplete data on the need for TCP.
Study variables
The variables analyzed were:
• Age - the average age calculated and also divided into groups for analysis: less than 60 years and greater than or equal to 60 years;
• Gender (male/female);
• Left ventricle ejection fraction (EF) - calculated by echocardiography, shared values for analysis in less than 40% and greater than or equal to 40%;
• Chronic kidney disease (CKD) - diagnosed by serum creatinine> 1.5 mg/dl;
• Diabetes mellitus (DM);
• Chronic obstructive pulmonary disease (COPD) - diagnosed clinically and/or radiological examination and / or spirometry and / or drug therapy (corticosteroids, bronchodilators);
• Atrial fibrillation (AF);
• Previous Heart surgery (CVS);
• Previous use of antiarrhythmic drugs (propafenone, and/ or amiodarone);
• Previous use of beta-blockers;
• Previous use of digoxin;
• Class functional New York Heart Association (NYHA);
• Type of cardiac procedure: mitral valve, aortic valve, including valve associated with CABG surgery and combined valve (aortic + mitral);
• Type of prosthesis (biological or metallic);
• Calcification;
• Time of cardiopulmonary bypass (CPB);
• Time of aortic clamping;
• In-hospital mortality.
Outcome
Development of AVB in the POCS and the need for TCP and definitive.
Procedures
Anesthesia, the techniques of CPB and cardioplegia were performed according to the standardization of the Hospital São Lucas da PUC-RS, as previously described [4]. After surgery, all patients were transferred to the ICU postoperatively in cardiac surgery, on mechanical ventilation.
Statistical analysis
The data were plotted on a Microsoft Access® spreadsheet and analyzed in SPSS Version 11.0. Descriptive statistics were performed, as well as the univariate tests: Chi-square for ordinal variables and was used for quantitative data analysis of variance or Student t test (for unpaired variables) followed by post hoc test for Bonferroni data.
Multivariate analysis was done by logistic regression (backward conditional method). Statistical difference was considered P <0.05.
Ethical considerations
The research project study was submitted to the Ethics Committee in Research of FAMED PUC-RS, under registration number 06003478.
RESULTS
Valve surgery from 1102 analyzed, 718 were aortic valve surgery, these 485 (67.56%), valve replacement for aortic stenosis, and 233 (32.45%), exchange for aortic insufficiency. Of the 407 mitral valve surgeries, 193 (47.4%) were mitral valve replacement and 214 (52.6%) for mitral regurgitation. One hundred and ninety (17.24%) surgeries were combined with CABG, these 143 (75.3%) aortic valve surgery (112 by aortic stenosis and 31 aortic) and 47 (24.7%) mitral valve surgery (14 by 33 by mitral stenosis and mitral insufficiency).
On total cardiac surgery and valvular aortic and/or mitral valve during the period analyzed, 187 (17.0%) patients had clinical and electrocardiographic atrioventricular block during the postoperative period, requiring TCP. Table 1 shows the profile of patients who required temporary pacemaker through TCP and univariate analysis of preoperative data of these patients compared with patients who underwent surgery and did not need the aforementioned device.
The characteristics of the patients are shown in Table 1: average age of 65.8 years (42% older than 60 years), the vast majority (90%) patients had an EF greater than 40%, 44% of cases had NYHA Class III and IV, 14% underwent previous cardiac surgery (CVS), 7% were taking antiarrhythmic medication, 25% beta-blockers and 32% digoxin, 7% were diabetic, 6.89% had chronic kidney disease (CKD) (serum creatinine greater than 1.5 mg/dl) and 20% had AF.
Evaluation of surgical risk score of Guaragna et al. [5] stratified the risk of patients studied in the following frequency: 36.7% of low risk, medium risk 33.7%, 16.6% high risk, 6.3% very high risk and 6.7% extremely high risk. Data analysis showed no statistical significance between the surgical risk of mortality and the need for TCP.
Univariate analysis, described in Table 1, revealed a greater need for TCP in POCS in patients over the age of 60 years (OR = 2.01, 95% CI 1.46 to 2.77, P <0.0001); CKD (OR = 2.12, 95% CI 1.26 to 3.58, P = 0.004), presence of AF (OR = 1.68, 95% 1.17 to 2.41, P = 0.004), antiarrhythmic drugs ( (OR = 2.03, 95% CI 1.22 to 3.38, P = 0.005), beta-blockers (OR = 1.66, 95% CI 1.18 to 2.33, P = 0.003) and cases of heart surgery (OR = 1.54, 95% CI 1.01 to 2.33, P = 0.04).
Table 2 shows the surgical characteristics of patients studied with univariate analysis of these data. About 187 surgeries requiring TCP, 111 (15.5%) had aortic valve surgery, 82 (43.8%) for aortic stenosis and 29 (15.5%) surgeries for aortic insufficiency, 83 (20. 4%) were mitral valve surgery, 40 of these (21.4%) for mitral stenosis and 43 (23%) for mitral surgery, seven (3.7%) by double replacement (aortic + mitral).
In this analysis, we observed a higher risk of TCP in POCS in patients undergoing mitral valve replacement (OR = 1.45, 95% CI 1.05 to 2.00, P = 0.02) and patients who received bioprosthetic (OR = 2.02, 95% CI 1.4 to 2.92, P <0.0001). The 198 patients who received bioprosthetic had higher average age (69.4 ± 13.1 years) compared to the population that did not use (52.3 ± 14.8 years). The 52 patients using prosthesis and required TCP greater mean age (74.1 ± 8.3 years).
Regarding importance, the occurrence of death in the POCS and the need for TCP showed no statistically significant association in univariate analysis (OR = 1.244, 95% CI 0.77 to 1.98, P = 0.361).
Conducted the data obtained from the multivariate analysis (Table 3) showed a significant association of AVB with mitral valve surgery (OR = 1.76, 95% CI 1.08 to 2.37, P = 0.002), implantation of a prosthesis biological (OR = 1.59, 95% CI 1.02 to 3.91, P = 0.039), age over 60 years (OR = 1.99, 95% CI 1.35 to 2.85, P <0.001), prior use of antiarrhythmic drugs (OR = 1.86, 95% CI 1.04-3.14, P = 0.026) and previous use of beta-blockers (OR = 1.76, 95% CI 1 0.25 to 2, 54, P = 0.002). Patients with AF, CKD and no prior CVS therefore presented significant risk for AVB in the POCS.
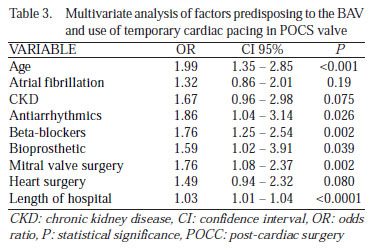
Multivariate analysis also revealed that the length of hospitalization was higher in patients requiring TCP by AVB, with a mean hospital stay was 13.59 days compared to 10.88 days who did not need TCP (OR = 1.03 95% CI 1.01 to 1.04, P <0.0001).
The subgroup of 187 patients with AVB and underwent TCP, 14 (7.5%) required implantation of DPM, accounting for 1.27% of the cohort analyzed. The average time from surgery to implantation of DPM was 11.33 days.
DISCUSSION
The TCP may be necessary in a post-operative cardiac intervention because of the manifest after the AVB procedure. They come as causes of the metabolic block, the residual effect of cardioplegia, edema, inflammation and bleeding near the conduction tissue, anoxia, support therapeutic drug, the iatrogenic injury of the conduction tissue and fibrosis. The AVB may provide temporary or permanent. There are no criteria that allow predicting the evolution of the blockade on its reversibility [6].
Patients who develop the AVB in the POCS generally require TCP and some of DPM to maintain hemodynamic stability and physiological parameters. In our study, incidence of AVB with TCP in 17% (187 cases) of the total of 1102 patients undergoing heart valve surgery during the period. However, most AVBs proved to be transient and reversible: only 1.27% of these patients developed DPM need to implant this hospital stay, incidence similar to the literature (1.3% to 9.7%) this association POCS [1-3,7-9].
There is an anatomical proximity to valve structures with the atrioventricular conduction system. Thus, we find reversible causes for AVB, and the most frequent local edema caused by surgical manipulation. This can cause temporary changes due to edema of the atrioventricular node, which can occur during surgery and provide spontaneous reversion hours or days after surgery. On the other hand, if there is direct injury of the conduction system (prolonged ischemia, damage by removal of calcium from the valve structures, or deep stitches, etc.) Disorder is expected to drive greater likelihood of permanent and irreversible [1-3].
Specifically, the association between mitral valve replacement surgery and AVB is still subject to debate, as well as the mechanism that produces [2,3]. The risk of using TCP these patients was 20.4 in this casuistic with statistical significance (OR = 1.76, 95% CI 1.08 to 2.37, P = 0.002). As already mentioned, the anatomy would be a relevant factor, especially the proximal part of the posterior commissure of the mitral valve structures of the conduction system. Gaudino et al. [10] and Garcia-Villarreal et al. [11] reported that 20% of patients who have replaced the mitral valve using the transseptal biatrial approach required DPM. This surgical approach would relate to the involvement of the sinus node artery before and internodal pathways. This technique, however, is rarely used in our service.
It is remarkable that in our series, aortic valve surgery, we found no increased risk of AVB in POCS. This finding differs from data in the literature, where no description of the incidence of AVB in up to 26%, and these cases need to DPM of 8.5% [7]. Still, these patients were reported factors, singly or in combination, could explain a potential increase in need for TCP [12,13]. The origin of the atrioventricular disorder may be the known age-associated aortic valve disease, mechanical factors (high pressure in the left ventricle), histological abnormalities in the conduction system, etc. Clinicopathologic study demonstrated that there is an area particularly at risk near the His bundle region comprised of non-coronary cusp and its portion adjacent to the right coronary artery [14].
The procedure used in bioprosthetic valve replacement also showed a statistically significant association in our analysis (OR = 1.59, 95% CI 1.02 to 3.91, P = 0.039). The average size (median value) in the service of the prostheses used for aortic valve replacement is 23 mm and the mitral valve, 29 mm, and all biological valves are valves used in the service supported. In the literature, is an analysis of type of prosthesis and the risk of permanent cardiac pacing for aortic valve replacement, in which the risk factors found in the type of prosthesis to prosthesis size was smaller than 21 mm [15]. A plausible relation to increased risk of TCP with bioprosthesis may be the type of implant used in older patients, since the age proved to be a risk factor for TCP.
The extent of coronary artery disease and the CPB time could compromise the myocardial protection during surgery, facilitating the ischemic injury and / or metabolic damage by the intrinsic properties of the atrioventricular conduction tissue (differs from cardiac myocytes and showed less tolerance to the effect of ischemia, to hyperkalemia, hypothermia and / or cardioplegia). Specifically, the use of cold potassium cardioplegic solution may cause temporary blockage of the conduction system [2]. These data were not confirmed in our analysis, where the CPB and aortic clamping were not associated with higher incidence of need for TCP.
Age older than 60 years represented a significant risk factor (OR = 1.99, 95% CI 1.35 to 2.85, P <0.001). The origin of this association is likely to encounter the known higher incidence of coronary obstructive component (possibly ischemic) associated with old age and also the fact that degenerative diseases of the conduction system are more frequent in this age group, increasing the likelihood damage to the conduction system and AVB [1,7,16,17].
The univariate analysis showed patients with prior CVS risk of AVB (22.7%). However, multivariate analysis did not confirm this relationship, perhaps by the small number of patients with this feature in our series. In the literature, the risk found for this subgroup is around 5.2% [17].
It is unclear the real role of antiarrhythmic drugs in an increased incidence of AVB in the POCS and the literature is conflicting [2,3]. In our group of patients, the preoperative use of propafenone and / or amiodarone (OR = 1.86, 95% CI 1.04 to 3.14, P = 0.026), as well as beta-blockers (OR = 1.76 95% CI 1.25 to 2.54, P = 0.002), proved to be a risk factor for AVB and need to TCP. We justify this association because this group of drugs able to produce pro-arrhythmic bradicardizanting effects and thus influence the normal function of the conduction system. Since the previous use of digoxin for patients undergoing valve surgery showed no risk. The long-acting beta-blockers such as atenolol are associated with higher incidence of blockages in the postoperative period [3].
As for other elements under review, both the CRD preoperatively for the presence of previous AF valvular surgery showed a trend, but without statistical significance, raising the risk of AVB in POCS.
The presence of AVB and need for TCP have not increased mortality in patients POCS valve (OR = 1.244, 95% CI 0.77 to 1.98, P = 0.361) but significantly prolong the hospital stay (P <0.0001) at the expense of longer hospitalization in the ICU (need to monitor clinical and hemodynamic restraint and care, among others) for the normal operation of the temporary pacemaker. This finding is relevant, since most patient's stay in ICU favors the emergence of infections and carries risks of prolonged immobilization [1,3,16,18].
The time elapsed after surgery safer and more necessary to indicate implant DPM remains uncertain [1]. The literature studies showing early implantation of the definitive pacemaker, as Berdajs et al. [3] who studied 391 patients in the period 1990 to 2003 who underwent mitral valve surgery and found an incidence of 4% of AVB in up to 4 days after surgery. In this work, we chose to deploy the DPM when the patient is able to be discharged from the ICU, and not wait for a week. Also the work of Kim et al. [18], we observe a similar behavior, where in a series of patients undergoing valve surgery that developed AVB in the first days after surgery, during long-term monitoring, found 56% of patients depending on cardiac pacing permanently. Thus, if the AVB is not resolved within 48 hours, recommended permanent pacemaker implantation up to five days, whereas, presumably, irreversible injury in the conduction system.
The Brazilian Guidelines for implantable devices, as well as the Consent to Permanent Cardiac Pacemaker Implant, and implantable defibrillators, recommends (class I level C) implantation of a cardiac stimulation device in patients with asymptomatic AVB, with wide QRS after heart surgery when persistent (> 15 days), AVB and consequent cardiac surgery, asymptomatic, persistent (> 15 days), with a narrow QRS or rhythm or nodal escape and good chronotropic response, or subsequent to cardiac surgery with no prospect of reversal (< 15 days) as class IIa, level C [19,20].
In the guideline of the American College of Cardiology/American Heart Association, the implementation of the DPM is indicated (class I, level C) for total AVB and AVB of the second advanced degree unresolved. The decision to deploy, as well as the wait interval, depends on the discretion of the treating physician [21].
Likewise, the directive of the European Society of Cardiology/Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy recommends (class I, level C) implantation of DPM in patients who develop complete atrioventricular block or second-degree Mobitz I or II after valve surgery, when it is not expected to resolve the blockade [22].
To meet these guidelines, decision-making in most implants performed in the patients, our policy to implant a permanent pacemaker is doing it in cases of AVB presumably irreversible, with an average of 11 days of POCS valve surgery. Conduct which is in agreement with the Brazilian guidelines (class IIa level of evidence C) and according to AHA / ACC and ESC (class I level of evidence C) [15-19].
The risk assessment used in this study is a score developed in the service of post-operative cardiac surgery at the Hospital São Lucas da PUC-RS, and has been validated in a previous study [5]. Although the EuroSCORE is the most widespread, their patient population differs from the Brazilian. The profile of patients undergoing cardiac surgery has changed compared to the 70, with the highest percentage of elderly and women, higher prevalence of poor cardiac condition and associated comorbidities [23]. In addition, only 30% of the EuroSCORE were valve surgery. We chose to use the score developed in the service.
CONCLUSION
This work highlights the risk factors associated with the development of AVB in POCS valve and the need for TCP. However, it should be noted that the potential risk of AVB does not significantly increase the mortality of these patients when undergoing heart valve surgery, but results in prolonged hospitalization.
This study shows the limitations of a retrospective study, although reflecting the "real world" of a large academic center. Within this limitation, we should mention the potential presence of non-measurable random variables because of the inherent lack of access to complete data. We must also take into account the results are from a single center series, which may represent some degree of bias in treatment. However, another factor to consider is the absence of definitive data as to the height of the atrioventricular conduction disturbance, escape rhythm, etc.
Still, the decisions of indication and the time of device implantation in our series were not uniform over time, which may have led to any deviation from the recommended guidelines on the subject [19-22].
Regarding the results of analysis of implant DPM, we found only a small number of patients who required the implantation of this device, making further analysis of data for this group of affected patients. However, the results for this group of patients are comparable to data in the literature [1-3,7,16,18].
REFERENCES
1. Merin O, Ilan M, Oren A, Fink D, Deeb M, Bitran D Permanent pacemarker implantation following cardiac surgery : indicatons and long-term follow-up. Pacing Clin Electrophysiol. 2009;32(1):7-12. [MedLine]
2. Meimoun P, Zeghdi R, D'Attelis N, Berrebi A, Braunberger E, Deloche A Frequency, predictors, and consequences of atrioventricular block after mitral valve repair. Am J Cardiol. 2002;89(9):1062-6. [MedLine]
3. Berdajs D, Schurr UP, Wagner A, Seifert B, Turina MI, Genoni M Incidence and pathophysiology of atrioventricular block following mitral valve replacement and ring annuloplasty. Eur J Cardiothorac Surg. 2008;34(1):55-61. [MedLine]
4. Guaragna JCV Cirurgia cardíaca e hipertensão arterial no pósoperatório imediato : fatores pré e transoperatórios1999;
5. Guaragna JCV, Bodanese LC, Bueno FL, Goldani MA Proposta de escore de risco pré-operatório para pacientes candidatos à cirurgia cardíaca valvar. Arq Bras Cardiol. 2010;94(4):541-8. [MedLine]
6. Nascimento CS, Viotti Junior LA, Silva LHF, Araújo AM, Bragalha AMLA, Gubolino LA Bloqueio atrioventricular de alto grau induzido pela cirurgia cardíaca : estudo de critérios de reversibilidade. Rev Bras Cir Cardiovasc. 1997;12(1):56-61. View article
7. Dawkins S, Hobson AR, Kalra PR, Tang AT, Monro JL, Dawkins KD Permanent pacemarker implantation after isolated aortic valve replacement : incidence, indications, and predictors. Ann Thorac Surg. 2008;85(1):108-12. [MedLine]
8. Del Rizzo DF, Nishimura S, Lau C, Sever J, Goldman BS Cardiac pacing following surgery for acquired heart disease. J Card Surg. 1996;11(5):332-40. [MedLine]
9. Lewis Jr JW, Webb CR, Pickard SD, Lehman J, Jacobsen G The increased need for a permanent pacemarker after reoperative cardiac surgery. J Thorac Cardiovasc Surg. 1998;116(1):74-81. [MedLine]
10. Gaudino M, Alessandrini F, Glieca F, Martinelli L, Santarelli P, Bruno P Conventional left atrial versus superior septal approach for mitral valve replacement. Ann Thorac Surg. 1997;63(4):1123-7. [MedLine]
11. García-Villarreal OA, González-Oviedo R, Rodríguez-González H, Martínez-Chapa HD Superior septal approach for mitral valve surgery : a word caution. Eur J Cardiothorac Surg. 2003;24(6):862-7. [MedLine]
12. Fukuda T, Hawley RL, Edwards JE Lesions of conduction tissue complicating aortic valvar replacement. Chest. 1976;69(5):605-14. [MedLine]
13. Davies M, Harris A Pathological basis of primary heart block. Br Heart J. 1969;31(2):219-26. [MedLine]
14. Gannon PG, Sellers RD, Kanjuh VI, Edwards JE, Lillehei CW Complete heart block following replacement of the aortic valve. Circulation. 1966;33(4):I152-61. [MedLine]
15. Elahi M, Usmaan K The bioprosthesis type and size influence the postoperative incidence of permanent pacemaker implantation in patients undergoing aortic valve surgery. J Interv Card Electrophysiol. 2006;15(2):113-8. [MedLine]
16. Gordon RS, Ivanov J, Cohen G, Ralph-Edwards AL Permanent cardiac pacing after a cardiac operation : predicting the use of permanent pacemarkers. Ann Thorac Surg. 1998;66(5):1698-704. [MedLine]
17. Koplan BA, Stevenson WG, Epstein LM, Aranki SF, Maisel WH Development and validation of a simple risk score to predict the need for permanent pacing after cardiac valve surgery. J Am Coll Cardiol. 2003;41(5):795-801. [MedLine]
18. Kim MH, Deeb M, Eagle KA, Bruckman D, Pelosi F, Oral H Complete atrioventricular block after valvular heart surgery and the timing of pacemarker implantation. Am J Cardiol. 2001;87(5):649-51. [MedLine]
19. Lorga AF, Fagundes AA, Barros ARC, De Paola AV, Pedrosa A, Grupi CJ Diretrizes Brasileiras de Dispositivos Cardíacos Eletrônicos Implantáveis (DCEI) : Sociedade Brasileira de Arritmias Cardíacas - SOBRAC/SBC, Departamento de Estimulação Cardíaca Artificial - DECA/ SBCCV. Arq Bras Cardiol. 2007;89(6):e210-37.
20. Kormann DS, Gauch PRA, Takeda RT, Andrade JCS, Galvão Filho SS, Greco OT Consenso para implante de marcapasso cardíaco permanente e desfibrilador - cardioversor implantável - 1995 : Departamento de Estimulação Cardíaca Artificial da Sociedade Brasileira de Cirurgia Cardiovascular. Rev Bras Cir Cardiovasc. 1995;10(2):107-14.
21. Epstein AE, DiMarco JP, Ellenbogen KA, Estes 3rd NA, Freedman RA, Gettes LS American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices); American Association for Thoracic Surgery; Society of Thoracic Surgeons : ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guidelines Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117(21):e350-408. [MedLine]
22. Vardas PE, Auricchio A, Blanc JJ, Daubert JC, Drexler H, Ector H Guidelines for cardiac pacing and cardiac resynchronization therapy : The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28(18):2256-95. [MedLine]
23. Cadore MP, Guaragna JCV, Anacker JFA, Albuquerque LC, Bodanese LC, Piccoli JCE Proposição de um escore em pacientes submetidos à cirurgia de revascularização miocárdica. Rev Bras Cir Cardiovasc. 2010;25(4):447-56. [MedLine]
Article receive on Thursday, May 26, 2011
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license