This study aims to verify the applicability of Ambler's risk score to patients who have undergone implantation of bovine pericardial bioprosthesis at the Instituto de Cardiologia do RGS/FCU. This study also aims to quantify the risk factors.
Retrospective study with 703 patients who had undergone implantation of bovine pericardial bioprosthesis between 1991 and 2005 at the Instituto de Cardiologia do RS. Aortic implant occurred in 392 patients, mitral in 250 and combined in 61. Primary outcome was hospital mortality. Characteristics used to estimate risk were: gender, age, body mass index (BMI), NYHA functional class, left ventricular ejection fraction, valvular lesions, systemic arterial hypertension, diabetes mellitus, renal function, cardiac rhythm, previous cardiac operations, and surgical priority. Univariate and multivariate logistic regression was used to quantify preponderant risk factors by the odds-ratio (OR).
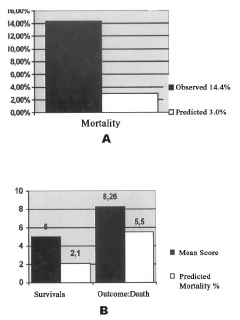
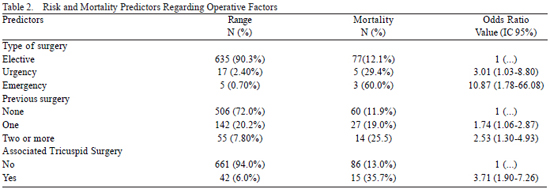
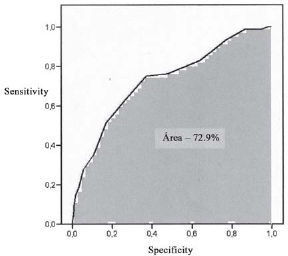
The mortality rate was 14.3%, which was higher than the estimated mortality rate (3%, according to Ambler's mean score of 6, (p<0.01)). Patients who died presented a mean score of 8.26, which was higher than the survivors' average score of 5.68. Characteristics of increased risk were emergency surgery (OR=10.87), dialysis (OR=6.10), and age higher than 80 years (OR=6.10). Our sample indicates an area under the ROC curve of 72.9% (accepted value > 70%).
The mortality predicted in Ambler's score was not reproduced in the observed results. However, the ROC curve provides evidence that this model is applicable. Preponderant risk factors were individualizated.
O estudo objetiva verificar aplicabilidade do escore de Ambler para pacientes que receberam implante bioprótese de pericárdio bovino no Instituto de Cardiologia do RGS/FUC e quantificar os fatores de risco.
Estudo retrospectivo com 703 pacientes submetidos ao implante de bioprótese de pericárdio bovino entre 1991 e 2005, no Instituto de Cardiologia do RS. Em 392 pacientes, ocorreu implante aórtico, em 250, mitral e, em 61, combinado. Desfecho primário foi mortalidade hospitalar. As características estimativas do risco foram: idade, sexo, IMC, classe funcional (NYHA), fração de ejeção ventricular esquerda (FE), lesão valvar, hipertensão arterial sistêmica, diabete melito, função renal, ritmo cardíaco, cirurgia cardíaca prévia, revascularização miocárdica e/ou plastia tricúspide concomitante, caráter cirúrgico. Utilizada regressão logística uni e multivariada para quantificar fatores de risco preponderantes, pelo odds ratio (OR).
A mortalidade observada foi de 14,3%, superior à prevista de valor 3% para escore médio 6 de Ambler, (p<0,01). Pacientes falecidos mostraram escore médio 8,26, superior ao dos sobreviventes, de 5,68. Características de maior risco foram cirurgia emergencial (OR=10,87), diálise (OR=6,10) e idade > 80 anos (OR=6,10). A área sob curva ROC para nossa amostra foi calculada em 72,9% (aceitável > 70%).
A mortalidade prevista no escore de Ambler não é reproduzida no resultado observado, mas a curva ROC evidenciou que o modelo é aplicável. Fatores de risco preponderantes foram individualizados.
INTRODUCTION
Valve replacement is the accepted treatment for serious defects with clinical repercussions or risk determinants, and has made favorable changes for the natural and clinical history of heart disease [1]. Among the available substitutes for implants, bioprostheses (homograft and bioprostheses) [2,3] are the most common, and offer advantages and disadvantages in long-term [4].
In addition to impacting in evaluations of late performance of a valve prosthesis, the surgical risk of implantation procedure has an important economic impact. It represents the technical quality of the surgical team, and decisively influences the recommendation of surgical intervention. This risk is little affected by the type of valve replacement [5,6], but is influenced by various demographic and operative factors, which are known to be able to affect immediate morbidity and mortality related to the procedure.
The creation of databases containing information about large numbers of patients operated in single or multiple centers allows for the development of risk scores for heart valve surgery [5] as well as other heart surgeries [7-10], and is similar to the EuroSCORE [11] and the Parsonnet [12]. These scores allow us to estimate the patient's individual immediate surgical risk. This information is important. It helps in recommendations for the procedure; it helps clarify things for the patient and their family, it is a resource for the surgical team, and it leads to more favorable outcomes by minimizing or neutralizing the indentified risk factors. However, the implementation of risk scores in medical centers different from where the data originated can lead to differing conclusions [5-13].
This study aims to verify whether the immediate surgical result in heart valve replacement with St. Jude-Biocor bovine pericardium bioprosthesis in patients operated at the Institute of Cardiology of Rio Grande do Sul meets the standard observed in the study of Ambler et al. [5], in order to gauge the score's validity in assisting in the management of patients to be operated in the institution. This study also hopes to quantify the influence of factors recognized as risk factors in the surgical procedure presented herein.
METHODS
Study Characteristics - Historical Cohort
Population
We included 703 patients who underwent implantation of at least one St Jude Medical-Biocor bovine pericardial bioprosthesis in the period from September 1991 to December 2005 at the Institute of Cardiology of Rio Grande do Sul. Among them, 359 were men and 344 were women. Their ages ranged between 17 and 88 years, with a mean of 62.5 years and standard deviation of ±17.2 years. The functional class, according to the standards of the New York Heart Association, was I in 19 (2.8%) patients, II in 151 (22.4%), III in 348 (51.7%) and IV in 155 (23.1%). Systemic arterial hypertension was found in 292 (41.5%) patients. Sixty-nine (9.8%) presented diabetes; 52 (7.5%) had a BMI less than 20 kg/m2 and 343 (49.8%) more than 25 kg/m2. The left ventricle ejection fraction was more than 50% in 512 (80.4%) patients, between 30 and 50% in 104 (16.3%) patients, and less than 30% in 21 (3.3%). Five hundred and thirty-two (75.7%) patients had preoperative sinus rhythm; atrial fibrillation was found in 152 (21.6%) patients, and atrioventricular block was found in 19 (2.7%). Serum creatinine was greater than 2.4 g/dL in 13 (1.8%) patients and 6 (0.8%) were on dialysis.
The criteria for surgical recommendation followed the established norms, as well as the recommendations for native valve replacement by bioprosthesis [14].
Valve replacement operation
The routines of the bioprosthesis implantation were performed under the operative and postoperative surgical care previously described [15]. The surgical procedures were performed with the use of a membrane oxygenator and under moderate hypothermia (32 to 28ºC) and myocardial preservation by hypothermic crystalloid cardioplegia.
Two hundred and fifty (35.6%) isolated implants of St. Jude Medical Biocor bioprosthesis in the mitral position and 392 (55.8%) in aortic position were performed; there were mitral-aortic bioprosthesis implants in 61 (8.6%) procedures. The valve replacement surgeries were combined with 158 (22.4%) procedures - either CABG procedures or correction of mechanical defects secondary to myocardial ischemia. The surgery was also combined with 42 (5.9%) procedures on the tricuspid valve. Regarding the type of surgery, 635 were elective, 17 urgent and 25 emergency surgeries, while 26 patients had not specified such information in their medical records.
Five hundred and six (72.0%) patients received a heart surgery. One hundred and forty-two had already undergone one heart surgery (20.2%) and 55 had already undergone two or more heart surgeries (7.8%).
After surgery, the patients were referred to the recovery room, where they received intensive care for at least 24 hours. The hospital discharge occurred after the 5th postoperative day, and the patients were not prescribed routine oral anticoagulant. Such treatment was recommended in the case of chronic atrial fibrillation, a greatly enlarged left atrium, or concomitant presence of mechanical prosthesis.
Outcomes and definition of risk factors
The primary outcome considered was death during hospital stay, after performing heart surgery, even if it occurred after more than 30 days after the surgery. The definition of the number of deaths allowed us to calculate the hospital mortality of the procedure, recognized as a real or observed mortality.
The characteristics of patients identified in this study met the criteria of Ambler et al. [5], which are:
Demographic characteristics: gender, age, cardiac arrhythmias, ejection fraction, systemic arterial hypertension, diabetes, BMI, renal failure (in case of serum creatinine ratio greater than 2.4 mg/dL and/or the performing of dialysis), functional class (according to the model proposed by the NYHA), type of valve lesion (aortic, mitral or mitral-aortic) and previous heart surgery.
Operative characteristics: time of surgery, associated surgery (CABG and tricuspid surgery), surgical valve reintervention and type of surgery (elective, urgent or emergency).
For each feature analyzed, a value was chosen. This value was established according the Ambler's score, and its sum corresponded to the individual score of each patient [5]. This value allowed for the calculation of a mean risk score for the entire population, and from this, to determine the predicted mortality for a given group of patients. Next, we compared the observed mortality and predicted mortality, and we expected no significant statistical difference that would represent the relevance of the score to the patients operated in the institution. For this calculation, Student's t test was used for non-paired samples and the significance level was considered an
a-critical of 5%. Odds ratio (OR) with confidence interval of 95% was obtained by means of logistic regression analysis in order to estimate the relative risk of each characteristic evaluated.
The ROC curve (Receiver Operating Characteristics Curve) was used based on the classification standards of the tested score. Calculating the area under curve was an indicator of the predictive value of the model proposed by Ambler.
Ethical considerations
For this study, a research project was submitted to the research unit of the Institute of Cardiology of Rio Grande do Sul and was approved for implementation by the Research Ethics Committee of the institution under the number 32043. Ethical norms concerning the privacy of patients and management of medical information have been met.
RESULTS
The mortality observed for the population included in the study was 14.3% and the predicted mortality by the Ambler's score was 3% (p<0.01). These values correspond, respectively, to scores of 12 and 6 (Figure 1A). Surviving patients showed a mean score of 5.68, corresponding to a predicted mortality of 3% (estimation of the score 6), whereas the patients who died showed mean score of 8.26 and predicted mortality of 5.5% (estimation of the score 8) (Figure 1B).
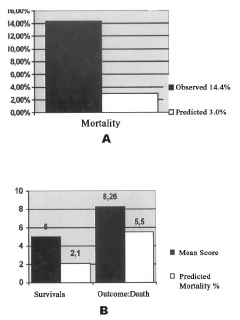
Fig. 1 - A: Predicted vs. Observed Mortality; B: Score vs. Predicted Mortality
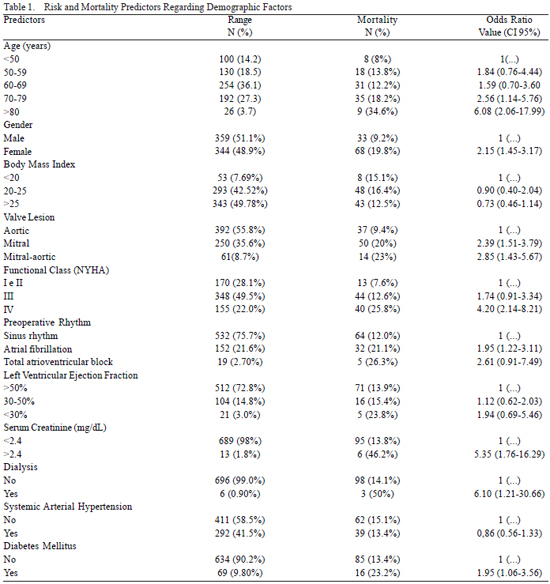
The odds ratio of the evaluated characteristics is shown in Tables 1 and 2 and in Figure 2. Higher values were observed for emergency surgeries (OR=10.87), dialysis (OR=6.10), age over 80 years (OR=6.10), creatinine greater than 2.4 mg/dl ( OR=5.35), IV functional class (OR=4.20), associated tricuspid surgery (OR=3.71), mitral-aortic lesion (OR=2.86), two or more previous heart surgeries (OR=2.53) and females (OR=2.43) (Tables 1 and 2, Figure 2).
The ROC curve resulting from this sample, shown in Figure 3, indicates an area under the curve of 72.9%.
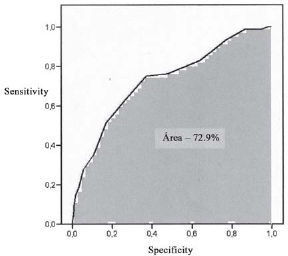
Fig. 3 - ROC Curve
The high number of valve replacement procedures performed annually, which is associated with a hospital mortality rate that ranges from 1 to 15% [5, 6] has led to a series of studies aiming to identify preoperative risk factors [16]. However, the variability of results has impaired the establishment of a risk prediction score that would allow surgeons to stratify the risk of each patient [10-13].
The base study of our research, presented by Ambler et al. [5], presents the following characteristics of risk stratification model for heart valve surgery: BMI, age, gender, type of valve lesion, CABG and/or tricuspid associated surgery, diabetes, renal failure, hypertension, arrhythmias, low ejection fraction, number of previous heart surgeries, and surgical priority. The choice of this score as a standard in establishing the risk of heart valve surgery was influenced by the fact that it includes the aforementioned characteristics. They are easily recognizable because they consider preoperative exam values, which are within the routines of the institution. This procedure has already been used in the institution for patients who have undergone CABG [17], using the same score used by the Cleveland Clinic [18].
In a study that examined 663 patients that underwent implantation of bovine pericardial bioprosthesis in mitral position from 1977 to 1988, Braile et al. [19] concluded that factors such as age and metabolic conditions of the patient, implant position and material and technical preparation of the valve to be implanted definitely affect the results and the durability of the prosthesis. These criteria for the recommendation of bovine pericardial bioprosthesis are comparable to those used in our institution, and the hospital mortality recorded was 9.2% - almost the same value recorded in our series.
In 2000, Hannan et al. [20] performed a study with 14,190 patients who had undergone heart valve replacement between 1995 and 1997, aiming to contrast the mortality with some demographic and operative characteristics and to better identify the risk factors. Mortality increased ninefold when preoperative cardiogenic shock was included a risk factor. Patients older than 55 years presented higher mortality, regardless of the type of heart valve replacement. Another relevant preoperative aspect was dialysis, and the patients who underwent the procedure presented increased mortality, with an OR of 9.37. Such a factor was also identified in the series presented herein.
Between September and December 1995, Nashef et al. [11] published the EuroSCORE, a predictor of hospital mortality for adult patients who have undergone various types of surgical valve procedures. The mortality observed for a total of 19,030 patients who had undergone valve replacement was 6.3% - lower than the mortality observed in the series we describe. The following were identified as characteristics significantly associated with high mortality: high age, creatinine levels, previous heart surgery, left ventricular function, congestive heart failure, pulmonary hypertension, endocarditis, emergency surgery, multiple valve replacement or tricuspid procedure, and concomitant CABG or associated thoracic surgery. These characteristics were similar to those found in this series - although the association with pulmonary hypertension, bacterial endocarditis and performance of the surgery of thoracic aortic portion has not been investigated.
In a study that included 8,943 patients between 1991 and 2001, Nowicki et al. [21] developed 11 characteristics connected to hospital mortality in aortic valve replacement: age over 70 years, small body surface, high creatinine levels, previous heart surgery, IV NYHA class, previous cardiac arrest, congestive heart failure, atrial fibrillation, emergency surgery, year of surgery and associated CABG. Their 10 statistically significant characteristics connected increased mortality in the case of mitral valve surgery were: female, elderly, diabetes mellitus, CABG, prior stroke, high creatinine levels, IV NYHA functional class, emergency surgery and congestive heart failure. Some of these factors were also related to increased mortality in the series described herein, and have already been reported [22].
The definition of odds ratios as a resource for statistical analysis has allowed us to estimate the surgical risk separately determined by one of the characteristics evaluated without interference from the others; it indicates that the hospital mortality could be reduced if the interference of other characteristics were removed or reduced [23]. The predictors of higher risk in this study were: emergency surgery (OR=10.87), dialysis (OR=6.10), age over 80 years (OR=6.10), creatinine level higher than 2.4 mg/dl (OR =5.35), IV functional class (OR=4.20), associated tricuspid surgery (OR=3.71), mitral-aortic lesion (OR=2.86), and two or more previous heart surgeries (OR=2.53).
Hellgren et al. [24] correlated the higher morbidity and mortality in heart valve replacement surgery in patients older than 70 years (OR=2.1), IV NYHA functional class (OR=2.2), preoperative cardiac arrest (OR of 3.5) and an aortic clamping time of more than 150 minutes (OR of 3.2). Atrial fibrillation was a significant operative risk factor when considered the type of valve procedure; in aortic or mitral-aortic replacements, it represented a risk factor with an OR of 4.1, but showed no relative influence on mitral replacements. According to the authors, the stratification of the potential risk predictor of each characteristic is best explained by the odds ratio, because it relates the influence that each analyzed characteristic has on the other.
The comparison between the findings of our analysis and those from Hellgren et al. [24] confirms emergency surgery, high age and class IV heart failure as predictors of higher operative risk. From these findings, we concluded that intervention in these factors - either by changing the criteria for surgical recommendation (making the decisions earlier), by creating better clinical protocol, or by changing operative routines - will allow us to achieve better results in terms of reducing surgical mortality and hospital expenses.
The ROC curve is the best method to establish the cut-off point; it optimizes the sensitivity and specificity of a diagnostic test. One of the advantages of this method is that the curves of different diagnostic tests can be compared, and the better the test is, the closer its curve will be to the upper left quadrant of the graph [25]. According to Swets [26], an area under the curve of less than 70% is related to satisfactory predictive values. Therefore, an area that corresponds to 72.9% - as identified in this study - makes the predictive power of our model clear.
In the surgical series presented herein, a comparison between mortality (14.3%) and predicted mortality (3%) by the score proposed by Ambler et al. [5] showed a statistically significant difference, but the analysis of the results using the ROC curve (area >70%) proved that this model of risk stratification is applicable to the patients of the institution. This study - when showing the predictors of operative risk - will allow for appropriate guidance regarding the management of specific patients in an attempt to reduce surgical morbidity and mortality.
REFERENCES
1. Birkmeyer NJ, Birkmeyer JD, Tosteson AN, Grunkemeier GL, Marrin CA, O'Connor GT. Prosthetic valve type for patients undergoing aortic valve replacement: a decision analysis. Ann Thorac Surg. 2000;70(6):1946-52. [
MedLine]
2. Wallace RB. Tissue valves. Am J Cardiol. 1975;35(6):866-71. [
MedLine]
3. Carpentier A, Dubost C, Lane E, Nashef A, Carpentier S, Relland J, et al. Continuing improvements in valvular bioprostheses. J Thorac Cariovasc Surg. 1982;83(1):27-42.
4. Jones El, Craver JM, Morris DC, King SB 3rd, Douglas JS Jr, Franch RH, et al. Hemodynamic and clinical evaluation of the Hancock xenograft bioprosthesis of aortic valve replacement (with emphasis on management of the small aortic root). J Thorac Cardiovasc Surg. 1978;75(2):300-8. [
MedLine]
5. Ambler G, Omar RZ, Royston P, Kinsman R, Keogh BE, Taylor KM. Generic, simple risk stratification model for heart valve surgery. Circulation. 2005;112(2):224-31. [
MedLine]
6. Jin R, Grunkemeier GL, Starr A; Providence Health System Cardiovascular Study Group. Validation and refinement of mortality risk models for heart valve surgery. Ann Thorac Surg. 2005;80(2):471-9. [
MedLine]
7. Ferguson TB Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL; STS National Database Committee. A decade of change--risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990-1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Society of Thoracic Surgeons. Ann Thorac Surg. 2002;73(2):480-9.
8. Grover FL, Shroyer AL, Hammermeister K, Edwards FH, Ferguson TB Jr, Dziuban SW Jr, et al. A decade's experience with quality improvement in cardiac surgery using the Veterans Affairs and Society of Thoracic Surgeons national databases. Ann Surg. 2001;234(4):464-72.
9. Ghali WA, Quan H, Shrive FM, Hirsch GM; Canadian Cardiovascular Outcomes Research Team. Outcomes after coronary artery bypass graft surgery in Canada: 1992/93 to 2000/01. Can J Cardiol. 2003;19(7):774-81. [
MedLine]
10. Tu JV, Jaglal SB, Naylor CD. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation. 1995;91(3):677-84. [
MedLine]
11. Nashef SA, Roques F, Michel P, Ganducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9-13. [
MedLine]
12. Parsonnet V, Dean D, Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79(6 Pt [part]2[/part]):I3-12. [
MedLine]
13. Kuduvalli M, Grayson AD, Au J, Grotte G, Bridgewater B, Fabri BM, et al. A multi-centre additive and logistic risk model for in-hospital mortality following aortic valve replacement. Eur J Cardiothorac Surg. 2007;31(4):607-13. [
MedLine]
14. Edmunds LH Jr, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Guidelines for reporting morbidity and mortality after cardiac valvular operations. The American Association for Thoracic Surgery, Ad Hoc Liaison Committee for Standardizing Definitions of Prosthetic Heart Valve Morbidity. Ann Thorac Surg. 1996;62(3):932-5. [
MedLine]
15. Braile DM. Preservação miocárdica. In: Nesralla I, ed. Cardiologia cirúrgica: perspectivas para o ano 2000. São Paulo:BYK;1994. p.264-82.
16. Scott WC, Miller DC, Haverich A, Dawkins K, Mitchell RS, Jamieson SW, et al. Determinats of operative mortality for patients undergoing aortic valve replacement. Discriminant analysis of 1,479 operations. J Thorac Cardiovasc Surg. 1985;89(3):400-13. [
MedLine]
17. Feier FH, Sant'Anna RT, Garcia E, Bacco F, Pereira E, Santos M, et al. The influence of time on the characteristics and risk factors for patients submitted to myocardial revascularization. Arq Bras Cardiol. 2006;87(4):439-45. [
MedLine]
18. Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992;267(17):2344-8. [
MedLine]
19. Braile DM, Ardito RV, Greco OT, Lorga AM. IMC bovine pericardial valve: 11 years. J Card Surg. 1991;6(4 Suppl):580-8. [
MedLine]
20. Hannan EL, Racz MJ, Jones RH, Gold JP, Ryan TJ, Hafner JP, et al. Predictors of mortality for patients undergoing cardiac valve replacements in New York State. Ann Thorac Surg. 2000;70(4):1212-8. [
MedLine]
21. Nowicki ER, Birkmeyer NJ, Weintraub RW, Leavitt BJ, Sanders JH, Dacey LJ, et al. Multivariable prediction of in-hospital mortality associated with aortic and mitral valve surgery in Northern New England. Ann Thorac Surg. 2004;77(6):1966-77. [
MedLine]
22. De Bacco MW, Sant'Anna JR, De Bacco G, Sant'Anna RT, Santos MF, Pereira E, et al. Fatores de risco hospitalar para implante de bioprótese valvar de pericárdio bovino. Arq Bras Cardiol. 2007;89(2):113-8.
23. Grunkemeier GL, Wu Y. What are the odds? Ann Thorac Surg. 2007;83(4):1240-4. [
MedLine]
24. Hellgren L, Kvidal P, Stahle E. Improved early results after heart valve surgery over the last decade. Eur J Cardiothorac Surg. 2002;22(6):904-11. [
MedLine]
25. Sackett DL, Haynes RB, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. 2nd ed. Boston:Litlle, Brown and Company;1991. p.370.
26. Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240(4857):1285-93. [
MedLine]

 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license