CLINICAL DATA
A 2-month-old female infant, with a birth weight of 3,390 g, prematurely born with a gestational age of 35 weeks and 2,200 g, recovered uneventfully until the first month, when she begun to demonstrate breastfeeding fatigue and cyanotic episodes. She had gastroesophageal reflux. She was clinically treated. Because there was no clinical picture improvement, the doctor ordered an echocardiogram. Upon a diagnosis of heart disease, furosemide and captopril were administered. She was referred to surgical treatment. She was in good general health, active, reactive, red-faced, hydrated, tachypneic, acyanotic, afebrile, and anicteric. The heart rhythm was regular with two normal clicks, with the hypophonetic second heart sound (S2), ejection systolic murmur ++/4+ in the left upper sternal border. Pulmonary auscultation was normal. There is no abdominal tenderness on palpation, with the liver 3 cm from the right costal margin. Because the increased amplitude in upper limbs and difficult to detect by palpation in lower limbs the pulses draw the attention.
ELECTROCARDIOGRAM
On electrocardiogram sinus tachycardia, heart rate of 166 bpm, ÂP + 60°, ÂQRS + 90º, PR interval = 0.08 seconds, QTc = 0.35 seconds, and signs of left atrium overload were all observed.
RADIOGRAM
On radiogram visceral situs solitus, cardiothoracic index of 0.61, discrete rectification of the costal arches and pulmonary vascular prominence with signs of pulmonary hyperflow, augmentation of the heart chambers, mainly the left atrium highlighted on lateral radiograph were all observed.
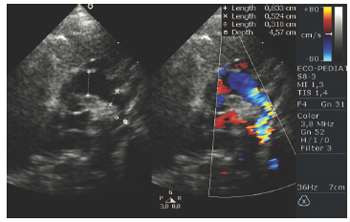
ECHOCARDIOGRAM
Situs Solitus was present at levocardia. Presence of a 12-mm aortopulmonary window (Figure 1); an 8-mm ascending aorta; a 5-mm aortic arch; and a 3-mm descending aorta in preductal region with an accelerated and turbulent flow in the descending aorta; and instantaneous gradient of 50 mmHg characterizing the aortic coarctation (Figure 2) were observed. Left atrium presented increased diameters, left coronary artery dilation with a 3-mm trunk and the right coronary artery with a 1-mm trunk.
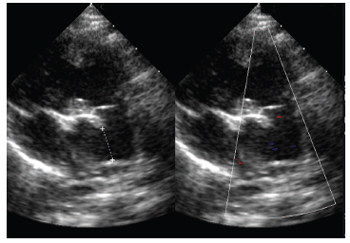
Fig.1 The Parasternal short axis two-dimensional echocardiogram, showing the communication between the pulmonary trunk (before the bifurcation of pulmonary branches) and the ascending aorta
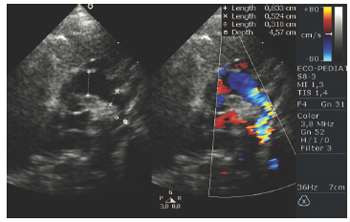
Fig.2 Color flow mapping echocardiogram on the longitudinal suprasternal section, showing the aortic arch with turbulence in the descending portion at the aortic coarctation site
The aortopulmonary window, when associated to other heart lesions, can be seen with an aortic arch interruption or an interventricular communication [1]. However, its association with the aortic coarctation is very uncommon. Color Doppler Echocardiography has clearly shown such a diagnosis and the indication to surgical repair in a single phase was chosen. On the differential diagnosis, it must be kept on mind the following: patent ductus arteriosus, truncus arteriosus, anomalous origin right pulmonary artery from ascending aorta, and the tetralogy of Fallot with pulmonary valve agenesis.
SURGERY
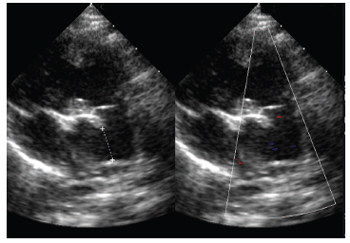
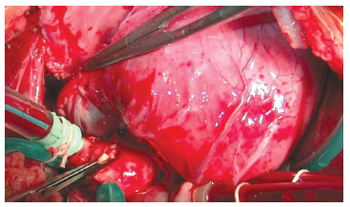
A longitudinal median sternotomy approach was performed, which facilitated the examination of the anatomical structures, giving an easy identification of the aortopulmonary window. (Figure 3) Cardiopulmonary bypass with cannulas in bicaval and aortic positions was established. A Profound hypothermia was initiated after the ligation of the pulmonary arteries. During the cooling-off period, an extensive dissection of the following structures: great vessels, aortic arch, and descending aorta. When the temperature reached 18ºC, hypoflow of 40 mL/kg, distal clamping of both aortic arch and descending aorta was performed. The aortic wall was largely resected in order to remove ductus arteriosus tissue, which had been previously resected. The coarctation was segmental; however, it was possible to perform a terminoterminal (end-to-end) anastomosis with an absorbable surgical suture 6-0. A normal flow was established, the descending aorta was clamped, antegrade cardioplegia was performed, with hypothermia 4ºC, and the repair of the aortopulmonary window was initiated with removal of pulmonary trunk flap to allow a greater amount of tissue to the aortic surface and the direct closing of the aortic wall where it was also employed the absorbable surgical suture. The pulmonary wall was repaired with a fresh autologous pericardium (Figure 4). The perfusion time was 93 minutes and myocardial ischemia was 25 minutes with a 12-minute hypoflow at 18ºC. The patient is recovering well in the immediate postoperative period using drugs for pulmonary hypertension. The postoperative echocardiogram showed an excellent surgical outcome with a discrete turbulence on Doppler at the aortic isthmus (gradient = 22 mmHg) without a clinical repercussion. The patient was discharged on the 14th day using captopril and diuretic.

Fig.3 The Baseline aspect externally highlighting the communication (window) existing between the descending aorta e the pulmonary trunk
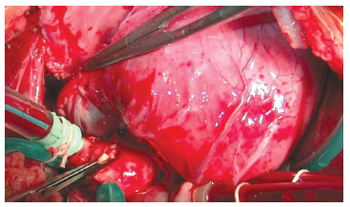
Fig.4 End aspect with the aortic surface reconstructed with a direct suture and the pulmonary surface with the fresh autologous pericardium
1. Konstantinov IE, Karamlou T, Williams WG, Quaegebeur JM, del Nido PJ, Spray TL, et al. Surgical management of aortopulmonary window associated with interrupted aortic arch: a Congenital Heart Surgeons Society study. J Thorac Cardiovasc Surg. 2006;131(5):1136-41.

 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license