Eucário Leite Monteiro ALVESI; Noedir Antonio Groppo StolfII; Ezequiel Cardoso Saraiva de ALMEIDAIII; Luiz Felipe Pinho MoreiraIV; Francisco Solano FEITOSA JÚNIORV; Paulo Sampaio GutierrezVI
DOI: 10.1590/S0102-76382006000300009
ABSTRACT
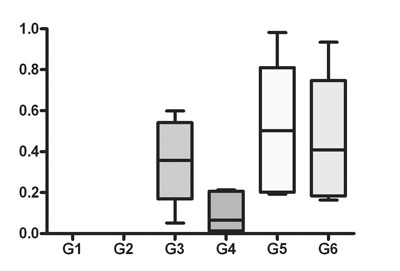
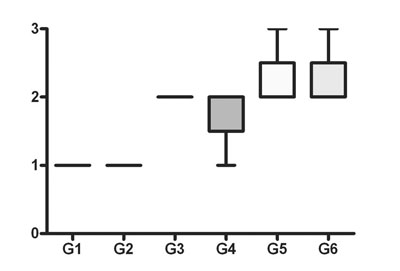
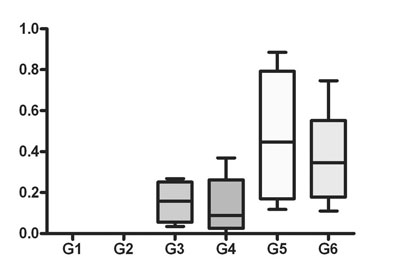
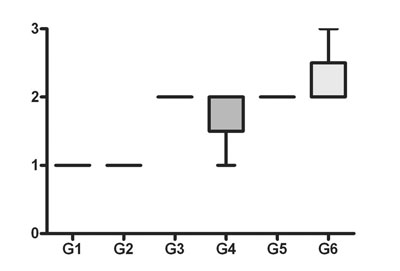
Objective: The purpose of this study was to assess the effect of CO2 on the wall of the Left Internal Thoracic Artery (LITA) and Anterior Interventricular Artery (AIVA) in an experimental model using goats, comparing the immediate effects of the use of CO2 at flow rates of 5 L/min and 10 L/min during 20 minutes, with intermittent flow (every 30 seconds) with and without humidification, simultaneously to the LITA and AIVA. Methods: Thirty-six male goats were submitted to a surgical procedure. Histological analysis was carried out using the immunoperoxidase reaction to mark the endothelium through the detection of VIII Coagulation Factor. Measurement was made by Quantimet following the Ip scale for vascular injury. Results: Within control groups, with and without humidification, both for AIVA and LITA, there was no endothelial injury. The flow rate of 5 L/min provoked moderately significant endothelial injury of the AIVA without humidification, whereas with humidification the endothelial injury was seen but without statistical significance. The flow rate of 5 L/min, with or without humidification, provoked insignificant endothelial injury at LITA. With a flow rate of 10 L/min, there was highly significant endothelial injury, both for the LITA and AIVA and whether humidified or not. Conclusions: In conclusion endothelial injury is flow-dependent with greater injury when using CO2 at a flow rate of 10 L/min and less at 5 L/min. The arteries involved in anastomosis (LITA and AIVA) are both affected, but there is a greater effect on the AIVA.RESUMO
Objetivo: O objetivo deste estudo é avaliar a influência do jato de CO2 na parede da Artéria Torácica Interna Esquerda (ATIE) e Artéria Interventricular Anterior (AIVA), em um modelo experimental em caprinos, comparando os efeitos imediatos do uso do CO2 com velocidade de fluxo de 5 L/min e 10 L/min, por 20 minutos, com fluxo intermitente (30 em 30 segundos), com e sem umidificação, simultaneamente nas ATIE e AIVA. Método: Trinta e seis caprinos foram submetidos ao procedimento cirúrgico. A análise histológica foi feita por meio da reação de imunoperoxidase para marcação do endotélio, por meio da detecção do Fator VIII da coagulação. A mensuração foi feita pelo Quantimet, seguindo a escala de Ip para lesão vascular. Resultado: Nos grupos controle, com e sem umidificação, não houve lesão endotelial. A velocidade de fluxo de 5 L/min provocou lesão endotelial com nível de significância intermediária na AIVA, sem umidificação; e, com a umidificação, a lesão ocorreu, porém, sem significância. A velocidade de fluxo de 5L/min, com e sem umidificação, provocou lesão endotelial na ATIE, contudo, sem significância. Com a velocidade de fluxo de 10 L/min, houve lesão endotelial com nível de significância importante, tanto para a ATIE quanto para a AIVA, não alterando se umidificado ou não. Conclusão: Pôde-se concluir que a lesão endotelial é fluxo-dependente. As artérias envolvidas na anastomose (ATIE e AIVA) foram afetadas simultaneamente, sendo que a agressão foi maior para AIVA .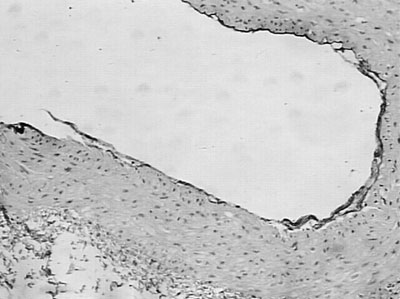
Article receive on Wednesday, March 1, 2006
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license