INTRODUCTION
Systemic lupus erythematosus (SLE) is an autoimmune disease with extremely varied clinical manifestations. The cardiovascular complications of SLE have been greatly studied over the last few years, as they are considered to be the third cause of mortality due to the disease, surpassed only by renal and infectious complications [1].
The most common cardiovascular presentation of SLE is pericarditis found in 62% of necrotic cases [2]. Other commonly seen forms are involvement of heart valves, which exhibit verrucous vegetations and myocardiopathy with incidences of 43% and 40% respectively.
Additionally, increases in the incidence of coronary disease associated to SLE have been registered over the last few years, whether due to lupus arthritis or the development of atherosclerosis. The occurrence of left ventricular aneurysms associated to SLE has been reported, to our knowledge, on only three occasions [3-5], justifying the current work.
CASE REPORT
The case of a 36-year-old female patient, who was accompanied for 10 years in the rheumatology outpatients' clinic with SLE, is reported. On July 12, 2002 she was admitted into the emergency department of the Agamenon Magalhães Hospital in Recife, Brazil, with clinical symptoms compatible with acute myocardial infarction: retrosternal pain, sudoresis, nausea, electrocardiographic alterations characterized by a positive deflection of the Q waves at DII, DIII and AVF and elevation of heart enzymes (CK 158, CK-MB 29 and troponin 16.7). An echocardiogram evidenced akinesia in the lower wall and an ejection fraction of 62%. She was clinically treated and remained in a stable state in the coronary unit. On July 20, 2002, the patient was submitted to a coronary cineangiography that demonstrated total occlusion of the middle one third of the right coronary artery. The other coronary arteries were normal. Ventriculography showed akinesia of the lower wall. The patient was released after 10 days in hospital and continued as an outpatient.
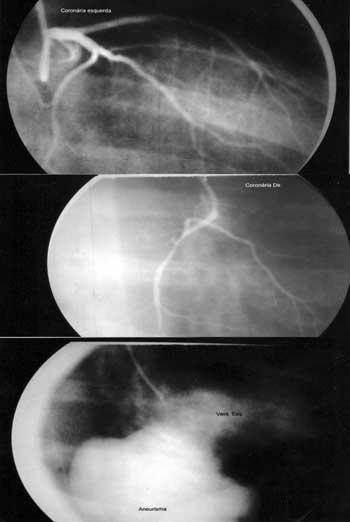
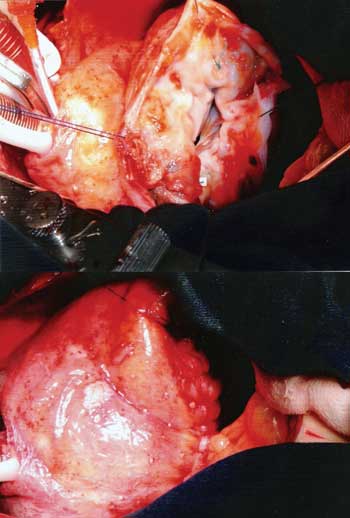
Progressively the patient evolved with severe heart failure, functional class IV - New York Heart Association. Another hemodynamic study revealed a pattern of the coronary arteries similar to the first study and the formation of an enormous aneurysm of the left ventricle lower wall (Figure 1). Surgical treatment was indicated. On January 8 2005, the patient underwent median sternotomy with conventional cardiopulmonary bypass at 32ºC and myocardial protection using an iced crystalloid cardioplegia solution at the aortic root and topical hypothermia of the heart. The aneurysm was opened and a large thrombus was removed. Repair of the heart was achieved with a linear suture anchored to a Teflon patch (Figure 2). The postoperative evolution was event-free and after four months of follow-up the patient remained asymptomatic from the cardiovascular point of view.
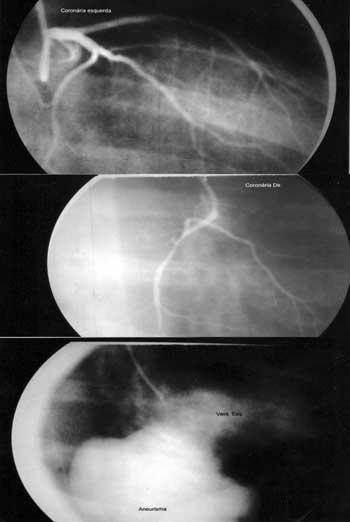
Fig. 1 - Coronary cineangiography showing a) obstruction of the right coronary artery and b) Normal left coronary artery. C) Left ventriculography showing the enormous aneurysm of the left ventricle lower wall
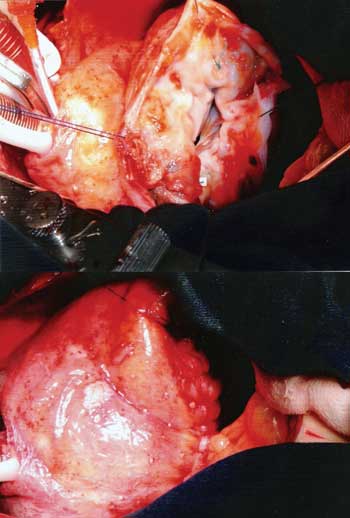
Fig. 2 - a) Open aneurysm b) Repair of the left ventricle by means of a primary suture
The development of myocardial infarction in young patients with SLE can result from arteriosclerosis that, sometimes, starts early as a result of the prolonged treatment with corticosteroids, due to hypertension and hypercholesterolemia, from coronary obstruction in lupus arteritis or from embolic phenomena in a previously normal coronary artery [1]. Independent of the cause of the infarction in SLE, the consequent appearance of a left ventricular aneurysm has been rarely described. The first case reported in the literature in 1993 was very similar to ours. It was related to a 30-year-old woman, who had angiographically normal coronary arteries and who probably suffered embolia of the anterior descending artery [3]. The resulting aneurysm was successfully treated surgically. Another case, was a small apical aneurysm of the left ventricle that appeared in the course of acute myocarditis due to SLE and improved with clinical treatment [4]. Finally, the third patient with SLE had established atherosclerosis, multiple coronary artery obstructions, a left ventricular aneurysm and aortic insufficiency [5]. The successful surgical repair consisted of aortic valve replacement and plicature of the ventricular aneurysm.
The current case demonstrates the rarity of the appearance of myocardial infarction and subsequent formation of a ventricular aneurysm in a patient with SLE and with previously normal coronary arteries. This case also calls the attention of the possibility of this type of event happening in the lupus population without history of cardiovascular diseases.
REFERENCES
1. Doherty NE, Siegel RJ. Cardiovascular manifestations of systemic lupus erythematosus. Am Heart J. 1985;110(6):1257-65.
2. Griffith GC, Vural IL. Acute and subacute disseminated lupus erythematosus: acorrelation of clinical and postmortem findings in eighteen cases. Circulation. 1951;3(4):492-500.
3. Nagaoka H, Funakoshi N, Innami R, Fugiwara A, Watanabe M. Left ventricular aneurysm, normal coronary arteries and embolization in a patient with systemic lupus erythematosus. Chest. 1993;103(1):287-8.
4. Frustaci A, Gentiloni N, Caldarulo M. Acute myocarditis and left ventricular aneurysm as presentations of systemic lupus erythematosus. Chest. 1996;109(1):282-4.
5. Giambuzzi M, Dottori V, De Gaetano G, Parodi E, Maccario M. Combined aortic valve replacement and left ventricular aneurysm plication in systemic lupus erythematosus. J Heart Valve Dis. 1996;5(2):228-30.
 All scientific articles published at bjcvs.org are licensed under a Creative Commons license
All scientific articles published at bjcvs.org are licensed under a Creative Commons license